Tendon transfers in irreparable ruptures of the posterosuperior rotator cuff. Latissimus dorsi and lower trapezius
Transferencias tendinosas en roturas irreparables del manguito rotador posterosuperior. Dorsal ancho y trapecio inferior
Resumen:
Las roturas masivas irreparables del manguito rotador posterosuperior son una de las patologías más desafiantes del hombro. El manejo de estas lesiones debe tener en cuenta las características del paciente, sus expectativas, el examen clínico, el número y la calidad de los tendones afectados.
Las transferencias tendinosas surgieron como opciones reconstructivas para reequilibrar el par de fuerzas anteroposterior en la articulación del hombro. Los principios de las transferencias incluyen que el músculo transferido sea prescindible, que la unidad músculo-tendón tenga una excursión similar, que la línea de tracción del tendón transferido y del músculo receptor sean similares en términos de fuerza biomecánica y que el músculo transferido reemplace al menos un grado de fuerza del músculo receptor deficiente.
Actualmente, se utilizan dos transferencias para el tratamiento de las roturas irreparables posterosuperiores del manguito rotador: la del tendón del músculo dorsal ancho y la de la porción inferior del trapecio. Ambas mejoran de manera uniforme la satisfacción del paciente, la elevación, la abducción y el rango de movimiento de rotación externa, pero con algunas peculiaridades que las diferencian.
Cuando consideramos realizar una transferencia tendinosa en una rotura masiva posterosuperior, el paciente debe haber agotado el tratamiento conservador, mantener una buena movilidad pasiva del hombro y comprender las expectativas postoperatorias y las posibles complicaciones.
El candidato ideal es un paciente activo y motivado, con mínimos cambios degenerativos de la articulación glenohumeral (Hamada grados 1 o 2), con una rotura irreparable del manguito con atrofia significativa, infiltración grasa y déficit funcional.
Las complicaciones de las transferencias tendinosas incluyen infección, hematoma, lesión nerviosa y fallo en la cicatrización o rotura tendinosa. Por lo tanto, se recomienda que estos procedimientos complejos sean realizados por cirujanos de hombro experimentados y que se realice una selección adecuada del paciente.
Abstract:
Irreparable massive rupture of the posterosuperior rotator cuff is one of the most challenging conditions of the shoulder. In the management of these lesions, consideration is required of the patient characteristics and expectations, the clinical examination, and the number and quality of the affected tendons.
Tendon transfers were introduced as reconstruction options to restore the anteroposterior balance of torque in the shoulder joint. The principles underlying transfer include the non-essential nature of the transferred muscle, similar excursion of the muscle-tendon unit, similar traction lines of the transferred tendon and the receptor muscle in terms of biomechanical strength, and the capacity of the transferred muscle to at least partially replace the strength of the deficient receptor muscle.
At present, two transfer strategies are used to treat irreparable posterosuperior rotator cuff ruptures: tendon of the latissimus dorsi muscle, and tendon of the lower portion of the trapezius muscle. Both techniques uniformly improve patient satisfaction and elevation, abduction and range of motion of external rotation, but with some differentiating particularities.
When considering tendon transfer in cases of massive posterosuperior rupture, the conservative management options must have been exhausted, with the maintenance of good passive mobility of the shoulder and due understanding of the postoperative expectations and possible complications.
The ideal candidate is an active and motivated patient with minimal degenerative changes of the glenohumeral joint (Hamada grades 1 or 2), and with irreparable cuff rupture with significant atrophy, fatty infiltration and functional deficit.
The complications of tendon transfer include infection, hematoma, nerve damage and healing failure or tendon rupture. It is therefore advisable for these complex procedures to be performed by experienced shoulder surgeons, and with adequate patient selection.
Introduction
Normal shoulder function depends on the combined action of the muscles of the rotator cuff and the deltoid muscle. These muscles act as dynamic stabilizers, centering the humeral head in the course of its movement(1). The forces that intervene in the glenohumeral joint act in pairs and are present in the coronal and the transverse planes(2). The balance in the coronal plane is maintained by means of torque involving the deltoid muscle and the lower cuff, while balance in the transverse plane is maintained by the subscapularis in the lower part and the infraspinatus and teres minor in the posterior part(3,4,5). Any imbalance in torque can alter the normal kinematics of the shoulder and cause loss of function. Tendon transfers were introduced as reconstruction options to restore the anteroposterior balance of torque in the shoulder joint.
Transfer of the latissimus dorsi
Anatomy and biomechanics
The latissimus dorsi is a triangular shaped muscle originating in the posterior portion of the iliac crest, the lumbar fascia, dorsal vertebras T7 to T12, the last four ribs, and in some cases the inferior angle of the scapula. The muscle in turn inserts in the bicipital groove of the humerus. It is innervated by the thoracodorsal nerve (C6-C8), and its function consists of extension, adduction and internal rotation of the arm(6).
Transfer of the tendon of the latissimus dorsi seeks to restore active external rotation of the shoulder in the context of imbalance caused by posterior cuff rupture(7). The first to use this transfer was L'Episcopo in 1936, for treating obstetric brachial paralysis(8). Posteriorly, Gerber used it successfully to treat irreparable massive rotator cuff ruptures(9,10). Transfer of the latissimus dorsi allows us to cover the posterosuperior defect and affords external rotation strength, thereby restoring torque and improving shoulder motion(11). With transfer to the most anterior zone of the greater tuberosity, the function of the latissimus dorsi switches from internal rotation to external rotation. This function is achieved by active muscle contraction but also through a tenodesis effect that exerts passive force to balance the torque. Furthermore, the latissimus dorsi acts as a humeral depressor, opposing its cranial displacement; this allows the deltoid muscle to be more efficient in abduction and anterior flexion of the shoulder(12).
However, despite the functional improvement achieved through transfer of the latissimus dorsi in irreparable posterior ruptures, normal external rotation function of the shoulder is not fully restored. This is mainly because the traction line of transfer of the latissimus dorsi is more vertical than that of the posterior cuff (infraspinatus and teres minor)(7).
Indications and contraindications of transfer of the latissimus dorsi
The success of any surgical technique is largely conditioned by a good indication, though in the specific case of tendon transfer due to irreparable cuff rupture, a good indication is crucial. The outcome can be influenced by many factors. Careful patient selection is therefore required, taking into account the indications and contraindications.
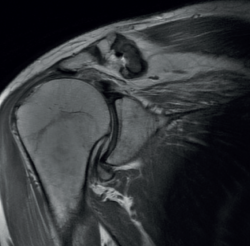
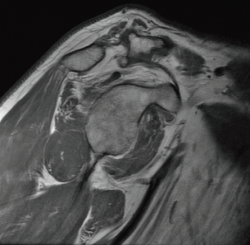
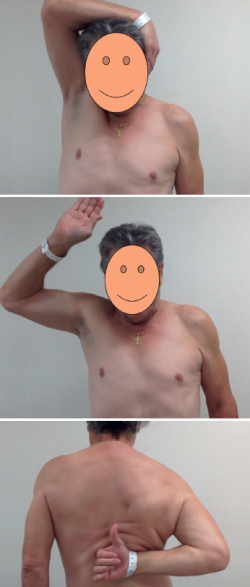
The preoperative evaluation must take a number of aspects into account, including patient age, pain, disability, functional demands and the patient expectations. In this respect, the patient must be duly informed about the expectable functional results. We also must consider other factors that can affect the surgical outcomes, such as patient comorbidities, deltoid muscle and subscapularis function, the integrity of the coracoacromial arch, the presence of arthrotic changes (Figure 1), and the need for the patient to enter prolonged rehabilitation. The main symptoms of massive ruptures of the rotator cuff are typically pain, weakness and loss of mobility(13,14). Irreparable massive ruptures are a common cause of intense pain and often prove extremely disabling for the patient. In general, patients with posterosuperior cuff rupture present reduced flexion-elevation and abduction, and total or partial loss of active external rotation(15,16). A positive external-rotation lag sign and positive hornblower sign are indicative of a deficit of the posterior cuff with the disabling of external rotation, and are associated with irreparable rupture of the teres minor and advanced fatty infiltration(17,18). The appearance of these signs at exploration is associated with poor outcomes of transfer of the latissimus dorsi(13,19). Weakness proves highly variable, and in extreme degrees we observe pseudo-paralysis. Although consensus is lacking, pseudo-paralysis in elevation could be defined as the inability to perform active flexion-elevation of 90º in the absence of nerve damage and with preserved passive mobility. External rotation pseudo-paralysis is defined as the complete loss of active external rotation strength in the presence of unrestricted passive external rotation and the absence of neurological lesions. Some authors consider pseudo-paralysis to be a contraindication to transfer of the latissimus dorsi(20), and is seen to be associated with poor outcomes, since it does not afford the necessary strength to overcome a pseudo-paralytic shoulder and achieve postsurgical elevation(12). Most authors agree that the deltoid muscle must be in good condition in order to perform transfer(21). Irreparable rupture of the subscapularis is an absolute contraindication to this kind of transfer, due to anterior escape of the humeral head when the deltoid muscle contracts in the absence of the subscapularis(9). However, good results can be obtained in partial ruptures of the upper third of the subscapularis that can repaired in the same surgical step(21) (Figures 2 and 3).
The presence of severe osteoarthrosis, above Hamada stage 2(22), or the existence of anterosuperior escape, is considered to be a contraindication to transfer, since both are associated with poor outcomes in transfer of the latissimus dorsi(23,24).
The absolute contraindications are:
- Deltoid muscle paralysis.
- Advanced glenohumeral osteoarthrosis (Hamada 3, 4 or 5).
- Infection.
- Irreparable subscapularis rupture.
- Pseudo-paralysis with elevation < 90º.
- Anterosuperior escape.
The relative contraindications are:
- Elderly patients.
- Fatty infiltration of the teres minor.
- Subscapularis repair under tension.
- Poor bone quality.
- Deficient patient commitment to postoperative rehabilitation.
Surgical technique
Transfer of the latissimus dorsi can be made via an open technique (with double or single incision) or in combination with arthroscopy.
Double incision
The original technique described by Gerber involved a double incision through the axilla for deinsertion of the tendon and superiorly through the deltoid muscle for deinsertion of the latter(9). The operation is carried out with the patient in lateral decubitus. A superior approach is adopted, with a medial incision parallel to the lateral acromion, separating the middle deltoid with a small fragment of the lateral acromion, which allows us to expose and partially repair the rotator cuff, associated to reinsertion of the latissimus dorsi. The axillary approach is performed with the arm in full elevation, through an L-shaped incision at the anterolateral margin of the latissimus dorsi. The latissimus dorsi is located anterior to the teres major, and its tendon is broad and very thin. We dissect the interval between these two muscles and free the insertion in the humerus. Once freed from the humeral insertion, the tendon is reinforced with two high-resistance sutures in Krackow configuration, to prevent possible tearing. Then, the muscle belly is dissected, identifying the neurovascular pedicle to increase mobility. The muscle is transferred through the interval between the deltoid muscle and the infraspinatus and teres minor. The tendon is then fixed in the insertion of the supraspinatus with anchorings, while fixation of the remaining rotator cuff is performed to the medial margin of the tendon. The middle deltoid muscle is repaired in the lateral acromion using transosseous sutures.
Single incision
A less invasive technique is the posterior single incision approach described by Habermeyer(25). The main advantage of this technique is that the deltoid muscle is not deinserted, and the posterior rotator cuff is directly visualized through a V-shaped posterior incision. The main disadvantage is that the anterosuperior rotator cuff cannot be visualized or repaired when necessary. The site of transfer fixation is somewhat more posterior and lateral, in the insertion footprint of the infraspinatus.
Arthroscopy-assisted technique
The technique can be carried out assisted by arthroscopy(26,27) or adopting a fully arthroscopic approach(28), thereby avoiding the damage to the deltoid muscle that may occur during open transfer. With the arthroscope in the posterior portal, we prepare the anterior and lateral portion of the greater tuberosity in the footprint of the supra- and infraspinatus for fixation of the latissimus dorsi. Then, with the arthroscope in the lateral portal, passage between the deltoid muscle and teres minor is established with the synoviotome and vaporizer. We then perform dissection and preparation of the latissimus dorsi through an axillary approach. Next, the tendon is passed between the deltoid muscle (superficial) and the infraspinatus and teres minor (deep), pulling upon the sutures through the anterior portal, and finally fixing the tendon with anchorings.
A mini-open approach was posteriorly introduced for deinsertion of the latissimus dorsi that was used in combination with arthroscopy for transfer and fixation(29). The pedicle of the latissimus dorsi is identified preoperatively by doppler ultrasound, allowing us to perform a minimal axillary incision of about 5 cm with simple dissection, thereby reducing the length of the incision. Tendon fixation is performed via arthroscopy.
Postoperative phase
Immediately after the operation, the shoulder is fitted with an abduction splint for 6 weeks. Postoperative physiotherapy starts from the first day, performing only passive mobilization during these first 6 weeks. The abduction splint is removed after 6 weeks and active mobility is started. After three months, gradual strengthening exercises are started, and after 6 months unrestricted strengthening exercises can be introduced.
Results
According to Gerber(13), pain, mobility and function improved after the open surgical technique. Seventy-four percent of the patients considered the outcome to be good or excellent at 10 years, and most of them reported high degrees of satisfaction and a willingness to undergo the surgery again. In this study, the patients presented a postoperative mean subjective shoulder value (SSV) of 70%, and active external rotation improved 18º to 30º. In addition, active elevation improved significantly at 10 years of follow-up, with an average of over 120º. Thirty-two patients presented an increase in SSV of over 30%, and only 14 patients had an increase in SSV of less than 30%, considering the outcome to be unsatisfactory. Those patients with a poor outcome had more fatty degeneration of the teres minor, and a higher incidence of subscapularis insufficiency and of latissimus dorsi muscle inactivation. Despite the important improvements observed in terms of range of motion and pain, the gain in strength after tendon transfer is low: approximately 40% in women and 25% in men, in relation to the preoperative levels(13).
It has been reported that primary surgeries afford better results than revision surgeries(30). In addition, some authors have reported better outcomes in younger patients(24).
With regard to the surgical approach used, the literature offers no solid statistical data allowing valid comparisons to be made between single and double incision, though it has been reported that the results obtained with a single incision are comparable to those of the standard double incision technique. It has been reported that arthroscopy-assisted techniques afford results comparable to those of open transfer surgery(31).
Another factor that may influence the postoperative results is patient compliance and adherence to a strict physiotherapy regimen, needed to develop neuromuscular control for recruiting the latissimus dorsi as an external rotator instead of an internal rotator(32).
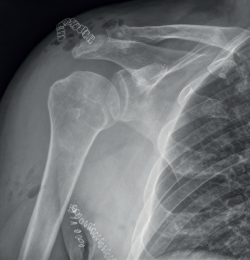
After transfer of the latissimus dorsi, arthrotic degeneration of the joint is comparable to that seen with non-surgical treatment, though progression is slower, and the increase is limited to 1 or 2 stages of the classification of Hamada(13) (Figures 4 and 5).
The incidence of complications of both the arthroscopic and the open techniques is low and includes postoperative hematoma, frozen shoulder, nerve damage, infection, and rupture of the transferred tendon(31).
Transfer of the lower trapezius
Traditionally, transfer of the latissimus dorsi has been regarded as the gold standard transfer in irreparable posterosuperior rotator cuff ruptures, and for several decades it has been used to treat these lesions, with good outcomes in terms of pain and function over the middle and long term.
Transfer of the lower trapezius was initially described for the treatment of brachial paralysis and paralytic shoulder, affording clear improvement in restoring external rotation in these patients(33,34,35). Based on these promising results, this type of transfer began to be used for treating irreparable posterosuperior rotator cuff rupture, employing the Achilles tendon as augmentation measure. At present, transfer of the lower trapezius has become consolidated as a very good treatment alternative in irreparable posterosuperior rotator cuff rupture, improving pain, range of motion and function of the shoulder(36).
The first results of transfer of the lower trapezius for treating massive posterosuperior rotator cuff rupture were published in 2016(37), with a mean follow-up of 47 months. In this study not only did the patients report improvements in terms of pain and range of motion, with an increase in the scores of all the applied scales, but recovery of function was also observed in patients with pseudo-paralytic shoulder.
Different biomechanical studies(38,39,40) have shown that transfer of the lower trapezius affords better leverage in external rotation than transfer of the latissimus dorsi, and is better able to restore the kinematics of the native glenohumeral joint. A recent biomechanical study has compared both transfers and has concluded that transfer of the lower trapezius is significantly better in preventing superior displacement of the humeral head and loss of mobility in abduction, compared with transfer of the latissimus dorsi(41).
However, few clinical studies have compared the two transfer techniques to date(42).
A recent study(43) has reviewed and compared patients subjected to transfer of the latissimus dorsi and transfer of the lower trapezius in irreparable posterosuperior ruptures. The authors see a potential advantage in the fact that the lower trapezius contracts during external rotation and abduction of the shoulder, in contrast to what happens with the latissimus dorsi, which is an internal rotator and abductor of the shoulder. This circumstance would allow better restoration of shoulder kinematics and better outcomes with the lower trapezius, as well as significantly contribute to stabilization of the scapula.
Another advantage of the lower trapezius versus the latissimus dorsi in relation to this transfer is its anatomy. The lower trapezius originates from the thoracic midline to T12, and inserts in the medial 4 cm of the scapular spine(44). Once transferred to the footprint of the supraspinatus, its traction line is very similar to that of the infraspinatus(45). In addition to its anatomical advantage, the trapezius is characterized by simple "learning" of its function once transferred, and this allows for faster recovery(46).
Nevertheless, transfer of the lower trapezius has two possible disadvantages. On one hand, augmentation with autograft or allograft is required, and this increases the costs, the surgery time and morbidity (in the case of autografts) of the process, and implies a risk of failure of graft fixation to the humerus and trapezius. On the other hand, deinsertion of the lower trapezius from the scapular spine could favor a degree of scapulothoracic dyskinesia.
Thus, due to its anatomy, its excursion and traction line much more similar to that of the infraspinatus, the lower trapezius has become the preferred option for many authors in treating massive posterosuperior ruptures, where the loss of external rotation is significant. In summary, according to these authors, the potential advantages of the lower trapezius versus the latissimus dorsi in application to irreparable rotator cuff ruptures are:
- A more cranial origin, with a traction line similar to that of the infraspinatus.
- Excursion and tension similar to that of the infraspinatus.
- The lower trapezius contracts during external rotation of the shoulder, acting as an agonist in external rotation(47).
Indications of transfer of the lower trapezius
The main objective of transfer of the lower trapezius is to restore flexion, external rotation and strength of the shoulder. The ideal patient in this respect is a young individual (under 65 years of age) with shoulder pain, loss of strength and active functional limitation in flexion and/or external rotation, with irreparable posterosuperior rotator cuff ruptures (with fatty infiltration of the supra- and infraspinatus corresponding to Goutallier grades 3-4), in the absence of glenohumeral osteoarthritis (Hamada < 3).
A number of doubts are raised regarding the indications and contraindications in certain clinical scenarios, and which we will address below in question-answer format.
Can transfer of the lower trapezius be made with a damaged subscapularis? Yes, provided the subscapularis can be repaired. Elhassan reported satisfactory outcomes in patients with a positive lift-off test and belly-press test on carrying out repair of the subscapularis and transfer of the lower trapezius(48,49,50).
Can transfer of the lower trapezius be made with a damaged teres minor? Transfer of the lower trapezius can be made with a damaged teres minor, though the outcomes are better if the latter muscle is preserved(48,51).
Can transfer of the lower trapezius be made with pseudo-paralytic shoulder? Elhassan et al.(33) recorded better results in patients starting from an anterior elevation of over 60º, with no glenohumeral osteoarthrosis or only minimal osteoarthrosis, and an evolution of under three years between symptoms onset and treatment. These authors consider that genuine pseudo-paralytic shoulder is a predictor of poor clinical outcomes. In this regard, genuine pseudo-paralytic shoulder is considered to be a shoulder with an anterior flexion deficit of less than 60º and abduction less than 60º during at least 6 months, with no improvement of range of motion after eliminating the pain through the infiltration of local anesthetic.
Thus, the absolute contraindications of transfer of the lower trapezius are:
- Paralysis of the lower trapezius.
- Active infection of the soft tissues or shoulder.
- The relative contraindications of transfer of the lower trapezius are:
- Pseudo-paralysis with elevation < 60º.
- Complete subscapularis rupture with superior escape of the humeral head.
One of the most important aspects to be taken into account when proposing transfer of the lower trapezius is that the patient must be convinced and motivated, as well as cooperative, since the postoperative period is long, with prolonged immobilization in external rotation for 6 weeks, and with a prolonged rehabilitation program. Patient failure to comply with such immobilization for 6 weeks will result in loss of tension of the plasty, and the functional outcomes probably will not be as desired.
It is also very important for the patient to strengthen the lower trapezius, as well as the rest of the periscapular muscles, before surgery is carried out. This will allow for optimum results. The patients are instructed to do external rotation against resistance exercises with the arm in adduction. A series of daily exercises during four weeks before surgery is enough.
One of the inconveniences of using the lower trapezius is that it needs a graft to reach the insertion. As a result, complications related to the graft could add to those inherent to the surgery itself. The allograft most often used in these transfers is the Achilles tendon. Some authors propose the use of a semitendinosus autograft instead of an Achilles allograft, in order to avoid the possible complications related to use of an allograft.
Surgical technique
The initial surgical technique described by Elhassan placed the patient in lateral decubitus, performing an osteotomy of the acromion to access the rotator cuff. The technique was subsequently modified, changing the patient to the deck chair position and adopting arthroscopic techniques for tendon reinsertion in the humerus - thus preserving the fibers of the deltoid muscle and avoiding osteotomy of the acromion. Arthroscopic tendon reinsertion has demonstrated better results than the classical open techniques; we therefore recommend its use in this type of transfer(42).
The surgical technique is described further on in another chapter of this monograph, so we will not address it in detail here.
During the postoperative period, the patient must keep the shoulder immobilized in external rotation with an orthosis for 6-8 weeks, and can only remove it for personal hygiene, maintaining the passive external rotation. From week six, assisted passive and active exercises are started, with a gradual increase in their intensity.
The possible complications of transfer of the lower trapezius are fundamentally two. The first, as already described by Elhassan(37), is the fact that some patients develop scapular dyskinesia following deinsertion of the lower trapezius from the scapular spine. The second complication is related to the fact that this is an indirect transfer, and thus the graft may fail at its insertion in the greater tuberosity, at middle level, or at its junction with the lower trapezius.
The technique is reproducible, with few complications, and is easier to perform than the latissimus dorsi procedure in obese patients. Furthermore, as also occurs with transfer of the latissimus dorsi, it may allow future reverse replacement if needed(27,52).
However, transfer of the lower trapezius is a relatively new technique, and long term studies are therefore needed to confirm the validity of the procedure. Comparative trials involving larger patient samples and longer follow-up periods are required to better understand the indications of this type of transfer as treatment for this disease condition.
Conclusions
Tendon transfers for the treatment of irreparable posterosuperior rotator cuff ruptures in patients with disabling loss of active external rotation, whether associated or not to loss of elevation of the shoulder, and without glenohumeral osteoarthritis, are demanding and complex procedures that can restore shoulder function and alleviate pain. In addition, they can help restore part of the strength, though this improvement should not be expected to be significant.
Candidate patients must be able to comply with long rehabilitation protocols and should be informed about the benefits to be expected after the operation. In this respect, the patient expectations must coincide with the predicted outcomes.
The long term failure rate is low and does not close the door to rescue surgery in the form or reverse replacement.
Careful patient selection is very important for the success of this surgery.
Figuras
Figure 2. Magnetic resonance imaging view of the same case. Coronal view showing retraction of the tendon stump to the glenoid cavity and fatty degeneration of the supraspinatus.
Figure 3. Sagittal view showing fatty degeneration of the supra- and infraspinatus, the good condition of the subscapularis, and hypertrophy of the teres minor.
Figure 4. Immediate postoperative view after transfer of the latissimus dorsi using the double approach.
Información del artículo
Cita bibliográfica
Autores
José Enrique Aroca Navarro
Hospital Universitari i Politècnic La Fe. Valencia
Marta Navarro Bosch
Hospital Universitari i Politècnic La Fe. Valencia
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that the procedures carried out abided with the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentiality. The authors declare that the protocols of their centre referred to the publication of patient information have been followed, and that all the patients included in the study have received sufficient information and have given written informed consent to participation in the study.
Right to privacy and informed consent. The authors have obtained informed consent from the patients and/or subjects cited in the article. The mentioned document is filed by the corresponding author.
Referencias bibliográficas
-
1Lippitt S, Matsen F. Mechanisms of glenohumeral joint stability. Clin Orthop Relat Res. 1993;(291):20-8.
-
2Burkhart SS. Fluoroscopic comparison of kinematic patterns in massive rotator cuff tears. A suspension bridge model. Clin Orthop Relat Res. 1992;(284):144-52.
-
3Burkhart SS. Arthroscopic treatment of massive rotator cuff tears. Clinical results and biomechanical rationale. Clin Orthop Relat Res. 1991;(267):45-56.
-
4Ahmad CS, Kleweno C, Jacir AM, et al. Biomechanical performance of rotator cuff repairs with humeral rotation: a new rotator cuff repair failure model. Am J Sports Med. 2008;36(5):888-92.
-
5Thompson WO, Debski RE, Boardman ND III, et al. A biomechanical analysis of rotator cuff deficiency in a cadaveric model. Am J Sports Med. 1996;24(3):286-92.
-
6Weening AA, Willems WJ. Latissimus dorsi transfer for treatment of irreparable rotator cuff tears. Int Orthop. 2010;34(8):1239-44.
-
7Omid R, Lee B. Tendon transfers for irreparable rotator cuff tears. J Am Acad Orthop Surg. 2013;21(8):492-501.
-
8L'Episcopo JB. Tendon transplantation in obstetrical paralysis. Am J Surg. 1934;25(1):122-5.
-
9Gerber C, Vinh TS, Hertel R, Hess CW. Latissimus dorsi transfer for the treatment of massive tears of the rotator cuff. A preliminary report. Clin Orthop Relat Res. 1988;(232):51-61.
-
10Gerber C. Latissimus dorsi transfer for the treatment of irreparable tears of the rotator cuff. Clin Orthop Relat Res. 1992;(275):152-60.
-
11Namdari S, Voleti P, Baldwin K, Glaser D, Huffman GR. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a systematic review. J Bone Joint Surg Am. 2012;94(10):891-8.
-
12Iannotti JP, Hennigan S, Herzog R, et al. Latissimus dorsi tendon transfer for irreparable posterosuperior rotator cuff tears. Factors affecting outcome. J Bone Joint Surg Am. 2006;88(2):342-8.
-
13Gerber C, Rahm SA, Catanzaro S, Farshad M, Moor BK. Latissimus dorsi tendon transfer for treatment of irreparable posterosuperior rotator cuff tears: long-term results at a minimum follow-up of ten years. J Bone Joint Surg Am. 2013;95(21):1920-6.
-
14Gerber C, Galantay RV, Hersche O. The pattern of pain produced by irritation of the acromioclavicular joint and the subacromial space. J Shoulder Elbow Surg. 1998;7(4):352-5.
-
15Boes MT, McCann PD, Dines DM. Diagnosis and management of massive rotator cuff tears: the surgeon’s dilemma. Instr Course Lect. 2006;55:45-57.
-
16Gerber C, Blumenthal S, Curt A, Werner CM. Effect of selective experimental suprascapular nerve block on abduction and external rotation strength of the shoulder. J Shoulder Elbow Surg. 2007;16(6):815-20.
-
17Hertel R, Ballmer FT, Lombert SM, Gerber C. Lag signs in the diagnosis of rotator cuff rupture. J Shoulder Elbow Surg. 1996;5(4):307-13.
-
18Walch G, Boulahia A, Calderone S, Robinson AH. The ‘dropping’ and ‘hornblower’s’ signs in evaluation of rotator-cuff tears. J Bone Joint Surg Br. 1998;80(4):624-8.
-
19Costouros JG, Espinosa N, Schmid MR, Gerber C. Teres minor integrity predicts outcome of latissimus dorsi tendon transfer for irreparable rotator cuff tears. J Shoulder Elbow Surg 2007; 16(6): 727-34.
-
20Nové-Josserand L, Costa P, Liotard JP, Safar JF, Walch G, Zilber S. Results of latissimus dorsi tendon transfer for irreparable cuff tears. Orthop Traumatol Surg Res. 2009;95(2):108-13.
-
21Warner JJ, Parsons IM. Latissimus dorsi tendon transfer: a comparative analysis of primary and salvage reconstruction of massive, irreparable rotator cuff tears. J Shoulder Elbow Surg. 2001;10(6):514-21.
-
22Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res. 1990:92-6.
-
23Debeer P, De Smet L. Outcome of latissimus dorsi transfer for irreparable rotator cuff tears. Acta Orthop Belg. 2010;76(4):449-55.
-
24El-Azab HM, Rott O, Irlenbusch U. Long-term follow-up after latissimus dorsi transfer for irreparable posterosuperior rotator cuff tears. J Bone Joint Surg Am. 2015 Mar 18;97(6):462-9.
-
25Habermeyer P, Magosch P, Rudolph T, Lichtenberg S, Liem D. Transfer of the tendon of latissimus dorsi for the treatment of massive tears of the rotator cuff: a new single-incision technique. J Bone Joint Surg Br. 2006;88(2):208-12.
-
26Gervasi E, Causero A, Parodi PC, Raimondo D, Tancredi G. Arthroscopic latissimus dorsi transfer. Arthroscopy. 2007;23(11):1243 e1-4.
-
27Marigi EM, Harstad C, Elhassan B, Sánchez-Sotelo J, Wieser K, Kriechling PJ. Reverse shoulder arthroplasty after failed tendon transfer for irreparable posterosuperior rotator cuff tears. Shoulder Elbow Surg. 2022 Apr;31(4):763-71.
-
28Cutbush K, Peter NA, Hirpara K. All-arthroscopic latissimus dorsi transfer. Arthrosc Tech. 2016;5(3):e607-13.
-
29Kany J, Kumar HA, Chang VK, Grimberg J, Garret J, Valenti P. Mini invasive axillary approach and arthroscopic humeral head interference screw fixation for latissimus dorsi transfer in massive and irreparable posterosuperior rotator cuff tears. Tech Shoulder Elbow Surg. 2010;11(1):8-14.
-
30Valenti P, Kalouche I, Díaz LC, Kaouar A, Kilinc A. Results of latissimus dorsi tendon transfer in primary or salvage reconstruction of irreparable rotator cuff tears. Orthop Traumatol Surg Res. 2010;96(2):133-8.
-
31Memon M, Kay J, Quick E, et al. Arthroscopic-assisted latissimus dorsi tendon transfer for massive rotator cuff tears: a systematic review. Orthop J Sports Med. 2018 Jun 11;6(6):2325967118777735.
-
32Donaldson J, Pandit A, Noorani A, Douglas T, Falworth M, Lambert S. Latissimus dorsi tendon transfers for rotator cuff deficiency. Int J Shoulder Surg. 2011;5(4):95-100.
-
33Elhassan B, Bishop A, Shin A, Spinner R. Shoulder tendon transfer options for adult patients with brachial plexus injury. J Hand Surg Am. 2010;35:1211-9.
-
34Elhassan B, Bishop A, Shin A. Trapezius transfer to restore external rotation in a patient with a brachial plexus injury. A case report. J Bone Joint Surg Am. 2009;91:939-44.
-
35Elhassan B. Lower trapezius transfer for shoulder external rotation in patients with paralytic shoulder. J Hand Surg Am. 2014;39:556-62.
-
36Duncan RP, Jobin CM, Chamberlain M, Numbari S, Tang CT, Galatz LM. Lower trapezius tendon transfer for irreparable postero superior cuff tear. Wahsington University Orthopedics, BJHospital, Saint Louis Poster AAO 2014.
-
37Elhassan BT, Wagner ER, Werthel JD. Outcome of lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tear. J Shoulder Elbow Surg. 2016;25:1346-53.
-
38Hartzler RU, Barlow JD, An KN, Elhassan BT. Biomechanical effectiveness of different types of tendon transfers to the shoulder for external rotation. J Shoulder Elbow Surg. 2012;21:1370-6.
-
39Omid R, Heckmann N, Wang L, McGarry MH, Vangsness CT, Lee TQ. Biomechanical comparison between the trapezius transfer and latissimus transfer for irreparable posterosuperior rotator cuff tears. J Shoulder Elbow Surg. 2015;24:1635-43.
-
40Reddy A, Gulotta LV, Chen X, et al. Biomechanics of lower trapezius and latissimus dorsi transfers in rotator cuff-deficient shoulders. J Shoulder Elbow Surg. 2019;28:1257-64.
-
41Muench LM, Berthold D, Kia C, et al. Biomechanical comparison of lower trapezius and latissimus dorsi transfer for irreparable posterosuperior rotator cuff tears using a dynamic shoulder model. J Shoulder Elbow Surg. 2022;31:2392-401.
-
42Woodmass JM, Wagner ER, Chang MJ, et al. Arthroscopic lower trapezius tendon transfer provides equivalent outcomes to latissimus dorsi transfer in the treatment of massive posterosuperior rotator cuff tears. J ISAKOS 2020;5:269-74.
-
43Baek CH, Lee DH, Kim JG. Latissimus dorsi transfer vs. lower trapezius transfer for posterosuperior irreparable rotator cuff tears. J Shoulder Elbow Surg. 2022;31:1810-22.
-
44Omid R, Cavallero MJ, Granholm D, Villacis DC, Yi AM. Surgical anatomy of the lower trapezius tendon transfer J Shoulder Elbow Surg. 2015;24:1353-8.
-
45Herzberg G, Urien JP, Dimnet J. Potential excursion and relative tension of muscles in the shoulder girdle: relevance to tendon transfers. J Shoulder Elbow Surg. 1999;8:430-7.
-
46Smith J, Padgett DJ, Dahm DL, et al. Electromyographic activity in the immobilized shoulder girdle musculature during contralateral upper limb movements. J Shoulder Elbow Surg. 2004;13:583-8.
-
47De Mey K, Cagnie B, Danneels LA, Cools AM, Van de Velde A. Trapezius muscle timing during selected shoulder rehabilitation exercises. J Orthop Sports Phys Ther. 2009;39(10):743-52.
-
48Elhassan BT, Alentorn-Geli E, Assenmacher AT, Wagner ER. Arthroscopic-assisted lower trapezius tendon transfer for massive irreparable posterior-superior rotator cuff tears: surgical technique. Arthrosc Tech. 2016;5:e981-8.
-
49Elhassan B, Sánchez-Sotelo J, Wagner E. Outcome of arthroscopically assisted lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tears. J Shoulder Elbow Surg. 2020;29:2135-42.
-
50Wagner ER, Elhassan BT. Surgical management of massive irreparable posterosuperior rotator cuff tears: arthroscopic-assisted lower trapezius transfer. Curr Rev Musculoskelet Med. 2020;13(5):592-604.
-
51Valenti P, Werthel JD. Lower trapezius transfer with semitendinosus tendon augmentation. Indication, technique, results Obere Extremität. 2018;13:261-8.
-
52Valenti P, Maqdes A, Werthel JD. Clinical and radiological outcomes after reverse shoulder arthroplasty in patients with failed deltoid or latissimus dorsi transfers. A review of ten cases. Int Orthop. 2017;41:2143-8.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Sometimes the rotator cuff injury of the shoulder is not repairable and we will have to do something with it…
- More manuscripts!
- Teach everything, tell everything
- Irreparable massive ruptures of the posterosuperior cuff: definition, diagnosis and classification
- Conservative management with medication and other non-surgical invasive therapies
- Physiotherapy and electrophysical therapies in the conservative management of irreparable posterosuperior rotator cuff rupture
- Alternatives in irreparable ruptures of the posterosuperior cuff. Debridement, tenotomy, partial repair
- Surgical alternatives in irreparable ruptures of the posterosuperior cuff
- Tendon transfers in irreparable ruptures of the posterosuperior rotator cuff. Latissimus dorsi and lower trapezius
- Reverse replacement in a patient without osteoarthritis
- Arthroscopic surgical technique for tendon transfer of the lower trapezius
- Arthroscopy assisted latissimus dorsi transfer for irreparable posterosuperior rotator cuff injuries really works
- Instructions for authors (Sept. 2023)
Más en PUBMED
Más en Google Scholar


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.