Evolution of spinal endoscopy. Where do we come from and where are we going?
Evolución de la endoscopia de columna. ¿De dónde venimos y a dónde vamos?
Resumen:
La endoscopia de columna lleva desarrollándose a pequeña escala desde los años ochenta, frenada por diversos factores, tales como la larga y compleja curva de aprendizaje, la falta de sistematización, el progresivo desarrollo tecnológico de materiales realmente apropiados para ello o la dificultad de transformar la práctica habitual de cirugía abierta en un campo tan delicado como la columna, por parte de cirujanos en activo habituados a trabajar con procedimientos tradicionales.
Sin embargo, desde el germen de la cirugía endoscópica que supuso la descripción del triángulo de Kambin como zona segura y su empleo para solo determinadas hernias discales, se ha pasado a convertir en rutina los accesos transforaminal e interlaminar hasta ser meras herramientas para propósitos mucho más complejos.
Del mismo modo, en la actualidad está próximo el establecer la endoscopia como gold standard para ciertos procedimientos sencillos como algunas hernias discales o estenosis, y ya son realidad técnicas como la fusión endoscópica por vía posterior, transfacetaria, foraminal, lateral o los procedimientos multiportal. Lo mismo ocurre con los accesos en la región cervical o dorsal, o su uso como técnica complementaria para otros procedimientos en el raquis y reducir su agresividad.
Abstract:
Spinal endoscopy has been developing on a small scale since the 1980s, hampered by a number of factors such as a long and complex learning curve, a lack of systematization, the gradual technological development of truly appropriate materials for performing the technique, or the difficulty of transforming routine open surgical practice in a field as delicate as the spine on the part of surgeons who are used to working with traditional procedures.
However, since the origin of endoscopic surgery with the description of Kambin's triangle as a safe zone and its utilization limited to certain disc hernias, transforaminal and interlaminar accesses are now routinely used to the point where they have become mere tools for much more complex purposes.
Likewise, at present, endoscopy is close to becoming the gold standard for certain simple procedures such as some disc hernias or stenoses, and techniques such as endoscopic fusion via the posterior, transfacet, foraminal or lateral route, or multi-portal procedures, have now become a reality. The same applies to accesses in the cervical or dorsal region, or utilization of the procedure as a complementary technique for other spinal operations, with the aim of reducing their aggressivity.
Introduction
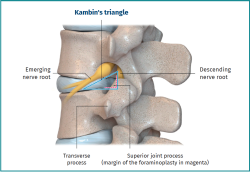
The discovery of Kambin's triangle in 1990 (Figure 1) offered the possibility of accessing the spine through the vertebral foramina safely and using endoscopy. This advance culminated in the transforaminal endoscopic technique, described in 1993 and developed in a rather inhomogeneous and less extended manner than open surgery assisted by translaminar endoscopy, and certainly much less than traditional open microdiscectomy.
reacae.30380.fs2209015en-figure1.png
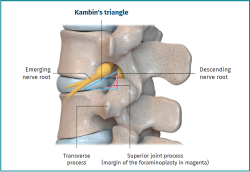
Figure 1. Schematic lateral view of Kambin's triangle and its anatomical relations. There is enormous anatomical variability that makes a greater or lesser foraminoplasty necessary in order to access the canal through it. As can be seen in the image, the limits of the triangle are the emergent nerve root, the descending root along with the margin of the superior joint process, and finally the margin of the inferior endplate to its junction with the lower pedicle.
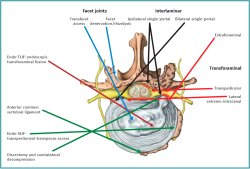
The development of percutaneous endoscopy has produced two fundamental systematic and differentiated approaches: transforaminal and interlaminar. However, endoscopy has moved far beyond these two approaches, which have become "tools" for more complex purposes ranging from all types of foraminal and canal decompressions to assistance in fusion procedures at any lumbar level, double or triple portals, or rescue of complications in previous surgeries (Figure 2).
reacae.30380.fs2209015en-figure2.png
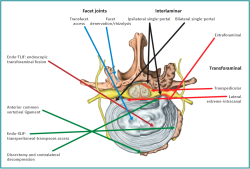
Figure 2. The range of different endoscopic accesses or approaches in the lumbar segment. The accesses moreover allowing assistance to lumbar fusion are shown in dark red, black and green. The direct approaches to the facetal joint, which currently limit use in performing endoscopic rhizolysis, are shown in light blue.
Accesses via endoscopy offer many advantages, including little or no infection, scant damage to the intermediate tissues, and amplified direct visualization of the operating zone. Nevertheless, it has limitations in terms of the operating field, conditioned by the need for initial planning of the access. This highlights the importance of especially thorough preoperative planning.
The present article addresses the more basic aspects of spinal endoscopy, its approaches and techniques, and discusses the consolidated indications - those which have already been implemented in daily practice - and the projections they may have in the context of spinal surgery in the future.
Spinal endoscopy techniques
The background, a historical reminder, and a description of the different endoscopic approaches are commented below.
Transforaminal approach
Endoscopic spinal surgery has experienced an important evolution in recent decades, from the percutaneous spinal approaches developed in the 1970s with Kambin and the first percutaneous nucleotomy performed by Hijikata(1) to so-called microsurgery towards the end of that decade. In the 1980s, this in turn gave rise to what we now know as endoscopic spinal surgery, starting with the transforaminal access through Kambin's triangle.
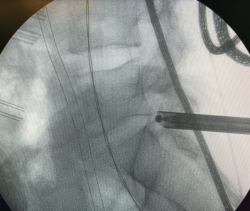
Starting in the 1980s and 1990s, Knight et al. introduced endoscopic spinal foraminoplasty with laser for performing decompressions at this level, considering it to be the safest technique for dealing with disc disease. This is because it does not alter the anatomy of the posterior spine, as there is no need for opening of the canal, laminectomy or flevectomy (Figures 3-5). Another advantage is reduction of the risk of damaging the dural sac and nerve roots. All this is due to the use of a natural orifice (vertebral foramen). The technique is widely used from T10 to L4-L5, though for levels L5-S1 access requires the combination of different techniques such as foraminoplasty of the lateral facet(2).
It would not be possible to understand endoscopic spinal surgery without the contribution of Kambin and his self-denominated triangle, described at around 1990. This zone is considered to be safe due to the absence of vascular or nerve structures that could be damaged, though there is controversy regarding description of the dimensions and limits of the triangle.
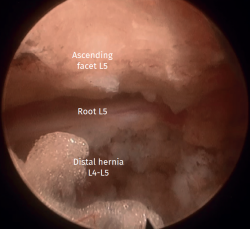
reacae.30380.fs2209015en-figure5.png
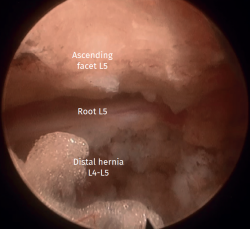
Figure 5. View from the optics of transforaminal endoscopy. This characteristic image of transforaminal endoscopy shows the ascending facet of the lower vertebra (at top in the image), the intersomatic space and the disc, the descending root and, in this case, also a hernial fragment under the root that will be extracted.
Kambin's triangle is a free space initially described at the outlet (or most lateral zone) of the vertebral foramen, caudad to the emerging nerve root. The base of this right triangle is the proximal platform of the body of the lower vertebra; its height is the ascending joint process of the lower vertebra, and the hypotenuse is the nerve root corresponding to that level, which emerges through the vertebral foramen (3).
The superior joint process was initially excluded from its definition, though this in fact is the most relevant structure to be taken into account. On the other hand, the concept was also expanded to comprise the so-called "Kambin's prism", in reference to the three-dimensional appearance of the structure due to its depth and shape on progressing through it towards the spinal canal. This concept became very relevant later on(4).
Initially, the structure was only considered to be relevant for extraforaminal disc hernias, with a stenotic foramen or canal becoming a poor prognostic factor and a contraindication for the technique. However, thanks to the great technological advances and the learning gained by surgeons, these contraindications are becoming obsolete, and all these scenarios are now considered to be open to endoscopic surgery(5).
Likewise, the development of this access route has made it possible to work along the entire vertebral foramen, even within the canal, ventral to the dural sac, until reaching the exit point of the contralateral vertebral foramen.
Moreover, the transpedicular approach has been described as a progression of the above, involving the creation of a tunnel through the pedicle to access the lateral recess at this level - this being difficult to do when entering through the foramen.
Translaminar or interlaminar approach
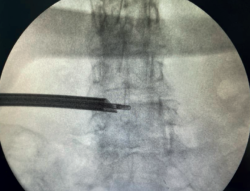
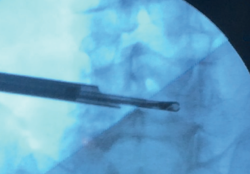
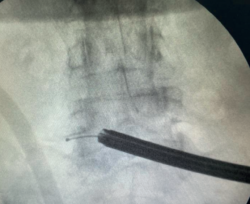
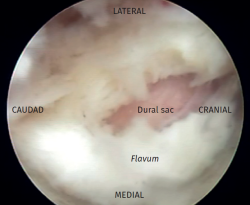
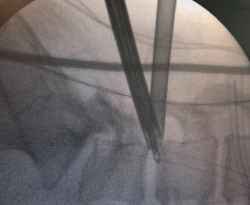
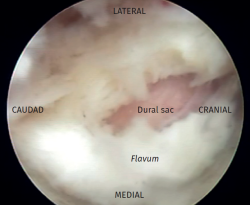
In the late 1990s(6) the first articles were published describing the translaminar approach to reduce the magnitude of bone resection. In contrast to the open technique, the endoscopic approach also reduces damage and removal of soft and muscle tissues(7). In 1995, Foley and Smith developed a technique for endoscopic hernia removal which they combined with the Love process through the interlaminar space, representing the natural evolution of the percutaneous technique used in previous years (Figures 6-9). Once within the space, the interlaminar window is expanded (if necessary), with partial removal of the ligamentum flavum to reach the canal and visualize the dural sac and nerve root(8).
Both approaches, transforaminal and interlaminar, have become perfectly complementary. Moreover, in contrast to classical spinal surgery, the percutaneous approaches, and specifically the endoscopic accesses, result in a smaller surgical wound (and therefore less damage to the intermediate planes), fewer infections, and a lesser risk of bleeding(9). In addition, the above is carried out under direct and precise visualization of the structures to be treated(10).
Although consensus on the part of the scientific community has not been reached, since utilization of the procedure has not yet been fully generalized, many authors already point to it as the new gold standard in discectomy for disc herniation(11,12).
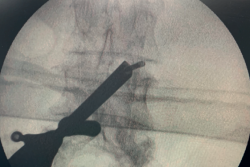
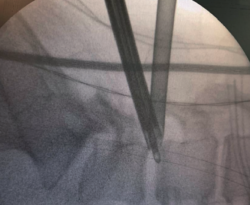
reacae.30380.fs2209015en-figure8.png
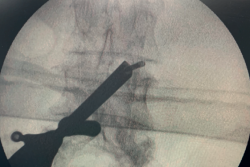
Figure 8. Radiological view of ipsilateral single-portal interlaminar endoscopy. In this technique the option of exploring the vertebral foramen (which in the open technique requires arthrectomy) was initially discarded; with the development of the procedure, exploring the foramen has also become technically possible.
At present, this is the most widely adopted approach, since it is the least invasive option, with lesser technical difficulty, and is more familiar to surgeons who previous employed open surgery. In addition, it can be performed with the patient in either prone or lateral decubitus(13).
This approach evolved rapidly, with an increase in the number of indications: disc hernias from L2-S1 (with or without displacement) to canal stenoses (whether central, lateral recess or foraminal) - with outcomes very similar to those of microsurgery but with fewer complications(2).
reacae.30380.fs2209015en-figure10.png
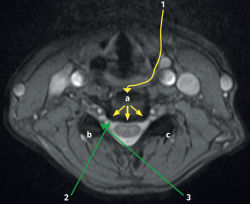
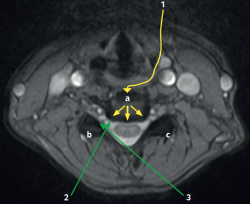
Figure 10. The different endoscopic approach options in the cervical spine. As can be seen, both are described, anterior and posterior. a: endoscopic anterior cervical approach; b: endoscopic posterior cervical approach, single-portal ipsilateral / foraminal; c: endoscopic posterior cervical approach, single-portal bilateral; 1: endoscopic anterior cervical approach; 2: single- or two-portal unilateral; 3: single- or two-portal bilateral.
Some initial studies have already been published on the use of this approach in thoracic and even cervical spine surgeries, which appear to be the next step in the evolution of endoscopy (Figures 10 and 11).
reacae.30380.fs2209015en-figure11.png

Figure 11. Endoscopic cervical decompression via the posterior approach. In the anatomical model, endoscopic access to the vertebral foramen is clearly seen, creating a tunnel that eliminates the posterior wall of the foramen, and allowing exploration of the emergence of the root and access to the disc.
Two-portal approaches
Both through the vertebral foramen and through the interlaminar window, it is possible to work with two portals if needed, in order to achieve the surgical objectives. Some groups, particularly in South Korea, postulate such two-portal accesses as a routine operating procedure(14,15).
Results
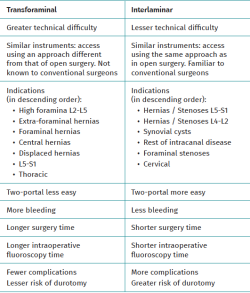
Comparison of the two techniques
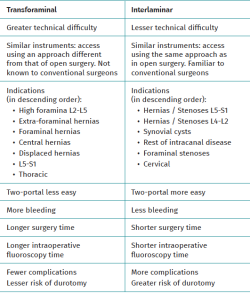
Both approaches make use of similar surgical material, including the two-portal techniques. Likewise, both approaches afford similar results in terms of recovery time in bed, hospital stay, clinical outcomes and reoperation rates. However, there are also some differences, as indicated in Table 1.
Jitpakdee et al. conducted a systematic review and meta-analysis comparing both techniques, with 1006 patients in the translaminar group and 942 patients in the interlaminar group. Similar results were obtained in terms of the Oswestry Disability Index (ODI) and visual analogue scale (VAS) (the scores being similar but better with the translaminar approach), patient satisfaction, hospital stay and complications. However, both surgery and scoping time were longer in the translaminar group, particularly at levels L5-S1(13).
Both approaches are very much conditioned by the learning curve, which classically has been regarded as very long. However, there are now some articles that comment on the possibility of shortening the curve when tutoring is performed by experts in endoscopic surgery. Some studies speak of the need for only 15 lumbar decompression cases in order to secure clinical outcomes similar to those of open surgery. In the study of Ramson, the variations in VAS scores proved statistically significant in both groups, though without significant differences between them (open laminectomy and endoscopic decompression). In turn, Gollogly reported a decrease in postoperative narcotics use after an initial learning curve of 15 patients(16). Likewise, there has been extensive discussion about the comparative technical difficulty of the two endoscopic approaches. Mayo et al., in a cohort of consecutive patients subjected to cervical anterior discectomy and fusion, found that 50% of the learning curve took place in cases 17 and 31, respectively, while 90% of the potential improvement was observed in cases 56 and 57, respectively - with a decrease in surgery time and blood loss, and higher arthrodesis rates(17).
Discussion and conclusions: the future of spinal endoscopy
Endoscopic spinal surgery has grown considerably in recent years, after a relatively slow start. At present it is fully developed, with an increase in the number of indications, and characterized by technological advances and a growing number of surgeons who have completed its long learning curve.
Among the aspects experiencing the greatest developments, mention must be made of cervical decompression and discectomy, transforaminal(18), transfacet, interlaminar or lateral intersomatic fusion, the possibility of obtaining disc biopsies, the removal of synovial cysts or certain tumors, or pure lateral endoscopic approaches that serve as a complement to the treatment of certain deformities.
The two-portal approach in spinal endoscopy is not only commonly used among surgeons who are already experienced with the technique but has also been described in many publications, particularly in countries such as South Korea. In this regard, the publication from the Hospital of Busan has made an extensive contribution(19,20) (Figure 12). Some studies have even reported greater clinical success with the two-portal technique than with the conventional microendoscopic approach(21). Success has also been recorded in tumor resection surgery, where the literature already describes the single-case removal of an extradural tumor using two portals, with complete tumor removal and no growth after one year of follow-up(22). Likewise, dura mater repair in ruptures occurring during endoscopy itself has been reported, though there is still considerable debate as to what type of treatment is needed(23).
Other less widely incorporated advances would be the treatment of areas of pain without mechanical problems amenable to more invasive treatment. This is thanks to the magnified vision afforded by endoscopy and the possibility of directly treating very small zones, as may occur in periradicular fibrosis(24).
A common feature of both approaches is the crucial need for prior surgical planning, though this may be more necessary with the transforaminal access or multiple accesses.
The prior imaging study allows us to select the correct site and entry angles, but is particularly useful for anticipating the anatomical incidents that may occur and which pose added difficulties during surgery.
Such planning, together with intraoperative tact of the endoscopy material, intraoperative fluoroscopy control, and the optics images, constitute the four cornerstones of the technique.
With regard to the learning curve, it must be noted that comparisons are made not only of the techniques or approaches, or between the endoscopic and the open techniques. Indeed, as these are endoscopic procedures, a clear distinction must be made regarding the type and difficulty of each technique in each case - a consideration not applicable to the same degree in open surgery. In order to assess these differences, both between the different results of the techniques and for assessing their learning curves, we consider that much more specific comparative studies are needed in reference to the type and location of the herniations, or the type and location of the stenoses.
Figuras
Figure 1. Schematic lateral view of Kambin's triangle and its anatomical relations. There is enormous anatomical variability that makes a greater or lesser foraminoplasty necessary in order to access the canal through it. As can be seen in the image, the limits of the triangle are the emergent nerve root, the descending root along with the margin of the superior joint process, and finally the margin of the inferior endplate to its junction with the lower pedicle.
Figure 2. The range of different endoscopic accesses or approaches in the lumbar segment. The accesses moreover allowing assistance to lumbar fusion are shown in dark red, black and green. The direct approaches to the facetal joint, which currently limit use in performing endoscopic rhizolysis, are shown in light blue.
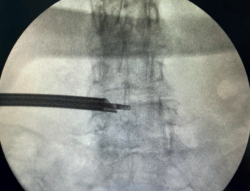
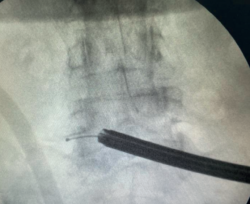
Figure 3. Radiological view of ipsilateral single-portal transforaminal endoscopy. As can be seen, the access allows easy reaching of the midline.
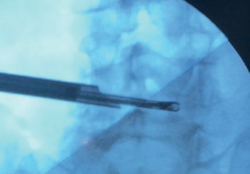
Figure 4. Radiological view of contralateral single-portal transforaminal endoscopy extending to the foramen, showing the capacity of endoscopy to treat contralateral disease in experienced hands.
Figure 5. View from the optics of transforaminal endoscopy. This characteristic image of transforaminal endoscopy shows the ascending facet of the lower vertebra (at top in the image), the intersomatic space and the disc, the descending root and, in this case, also a hernial fragment under the root that will be extracted.
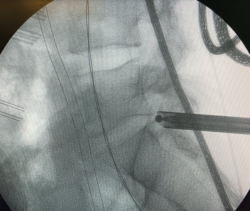
Figure 6. Radiological view of contralateral single-portal interlaminar endoscopy. Access through the contralateral interlaminar window and progress over-the-top to the contralateral recess, allowing the contralateral vertebral foramen to be reached and explored.
Figure 7. Radiological view of ipsilateral single-portal interlaminar endoscopy. The lateral view shows the trajectory of progression and the depth.
Figure 8. Radiological view of ipsilateral single-portal interlaminar endoscopy. In this technique the option of exploring the vertebral foramen (which in the open technique requires arthrectomy) was initially discarded; with the development of the procedure, exploring the foramen has also become technically possible.
Figure 9. View from the optics of interlaminar endoscopy. Ligamentum flavum opening phase. The image shows the ligamentum flavum with a loop through which the dural sac can be identified.
Figure 10. The different endoscopic approach options in the cervical spine. As can be seen, both are described, anterior and posterior. a: endoscopic anterior cervical approach; b: endoscopic posterior cervical approach, single-portal ipsilateral / foraminal; c: endoscopic posterior cervical approach, single-portal bilateral; 1: endoscopic anterior cervical approach; 2: single- or two-portal unilateral; 3: single- or two-portal bilateral.
Figure 11. Endoscopic cervical decompression via the posterior approach. In the anatomical model, endoscopic access to the vertebral foramen is clearly seen, creating a tunnel that eliminates the posterior wall of the foramen, and allowing exploration of the emergence of the root and access to the disc.
Figure 12. Ipsilateral two-portal interlaminar-transforaminal endoscopy. Radiological view of both cannulas located in the vertebral foramen to allow double instrument access.
Tablas
Información del artículo
Cita bibliográfica
Autores
Ricardo Casal Grau
Unidad de Raquis. Hospital Asepeyo Coslada. Madrid
Álvaro Ortega Carnero
Unidad de Miembro Inferior. Hospital Asepeyo. Coslada. Madrid
Unidad de Raquis. Hospital Asepeyo Coslada. Madrid
Manuel González Murillo
Unidad de Raquis. Hospital Asepeyo Coslada. Madrid
Pedro Estévez Sánchez
Unidad de Raquis. Hospital Asepeyo Coslada. Madrid
Jorge Omaña García
Unidad de Raquis. Hospital Asepeyo Coslada. Madrid
Javier Sánchez Benítez
Unidad de Raquis. Hospital Asepeyo Coslada. Madrid
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Khandge AV, Sharma SB, Kim JS. The Evolution of Transforaminal Endoscopic Spine Surgery. World Neurosurg. 2021 Jan;145:643-56.
-
2Yeung AT, Yeung CA. Advances in endoscopic disc and spine surgery: foraminal approach. Surg Technol Int. 2003;11:255-63.
-
3Montes García C. Endoscopia lumbar posterolateral con sistema YESS: reporte preliminar. Coluna/Columna. 2009;8(2):192-6.
-
4Fanous AA, Tumialán LM, Wang MY. Kambin's triangle: definition and new classification schema. J Neurosurg Spine. 2019 Nov 29:1-9.
-
5Ahn Y. Evolution of percutaneous endoscopic lumbar decompression. J Minim Invasive Spine Surg Tech. 2019;4:1-4.
-
6Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976). 2008 Apr 20;33(9):931-9.
-
7Oertel JM, Burkhardt BW. Endoscopic Translaminar Approach for Resection of Migrated Lumbar Disc Herniation. World Neurosurg. 2019 Aug;128:365.
-
8Dezawa A, Sairyo K. New minimally invasive discectomy technique through the interlaminar space using a percutaneous endoscope. Asian J Endosc Surg. 2011 May;4(2):94-8.
-
9Huang Y, Yin J, Sun Z, et al. Percutaneous endoscopic lumbar discectomy for LDH via a transforaminal approach versus an interlaminar approach: a meta-analysis. Orthopade. 2020 Apr;49(4):338-49.
-
10Telfeian AE, Veeravagu A, Oyelese AA, Gokaslan ZL. A brief history of endoscopic spine surgery. Neurosurg Focus. 2016 Feb;40(2):E2.
-
11Gatam AR, Gatam L, Phedy, Mahadhipta H, Ajiantoro, Aprilya D. Full Endoscopic Lumbar Stenosis Decompression: A Future Gold Standard in Managing Degenerative Lumbar Canal Stenosis. Int J Spine Surg. 2022 Sep;16(5):821-30.
-
12Muthu S, Ramakrishnan E, Chellamuthu G. Is Endoscopic Discectomy the Next Gold Standard in the Management of Lumbar Disc Disease? Systematic Review and Superiority Analysis. Global Spine J. 2021;11(7):1104-20.
-
13Jitpakdee K, Liu Y, Kotheeranurak V, Kim JS. Transforaminal Versus Interlaminar Endoscopic Lumbar Discectomy for Lumbar Disc Herniation: A Systematic Review and Meta-Analysis. Global Spine J. 2023 Mar;13(2):575-87.
-
14Choi DJ, Kim JE. Efficacy of Biportal Endoscopic Spine Surgery for Lumbar Spinal Stenosis. Clin Orthop Surg. 2019 Mar;11(1):82-8.
-
15Choi CM. Biportal endoscopic spine surgery (BESS): considering merits and pitfalls. J Spine Surg. 2020 Jun;6(2):457-65.
-
16Ransom NA, Gollogly S, Lewandrowski KU, Yeung A. Navigating the learning curve of spinal endoscopy as an established traditionally trained spine surgeon. J Spine Surg. 2020;6(Suppl 1):S197-S207.
-
17Mayo BC, Massel DH, Bohl DD, Long WW, Modi KD, Singh K. Anterior Cervical Discectomy and Fusion: The Surgical Learning Curve. Spine (Phila Pa 1976). 2016 Oct 15;41(20):1580-5.
-
18Zheng B, Shaaya E, Feler J, et al. Endoscopic Techniques for Lumbar Interbody Fusion: Principles and Context. Biomed Res Int. 2022 Mar 19;2022:4979231.
-
19Chu PL, Wang T, Zheng JL, et al. Global and Current Research Trends of Unilateral Biportal Endoscopy/Biportal Endoscopic Spinal Surgery in the Treatment of Lumbar Degenerative Diseases: A Bibliometric and Visualization Study. Orthop Surg. 2022 Apr;14(4):635-43.
-
20Choi DJ, Kim JE, Jung JT, et al. Biportal Endoscopic Spine Surgery for Various Foraminal Lesions at the Lumbosacral Lesion. Asian Spine J. 2018;12(3):569-73.
-
21Aygun H, Abdulshafi K. Unilateral Biportal Endoscopy Versus Tubular Microendoscopy in Management of Single Level Degenerative Lumbar Canal Stenosis: A Prospective Study. Clin Spine Surg. 2021;34(6):E323-E328.
-
22Kim SK, Bendardaf R, Ali M, Kim HA, Heo EJ, Lee SC. Unilateral Biportal Endoscopic Tumor Removal and Percutaneous Stabilization for Extradural Tumors: Technical Case Report and Literature Review. Front Surg. 2022 Mar 24;9:863931.
-
23Müller SJ, Burkhardt BW, Oertel JM. Management of Dural Tears in Endoscopic Lumbar Spinal Surgery: A Review of the Literature. World Neurosurg. 2018;119:494-9.
-
24Kim HS, Wu PH, Jang IT. Current and Future of Endoscopic Spine Surgery: What are the Common Procedures we Have Now and What Lies Ahead? World Neurosurg. 2020 Aug;140:642-53.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- From the start to the top: the history of knee osteotomies
- Clinical-functional and radiographic outcomes of medial valgus-producing tibial osteotomy
- Patellar tendinopathy: a practical consensus guide for choosing the best treatment
- Evolution of spinal endoscopy. Where do we come from and where are we going?
- Partial ruptures of the rotator cuff
- Arthroscopic core decompression of the femoral head with autologous stem cell placement as treatment for femoral head osteonecrosis
- Extraarticular plasty as sole maneuver in the correction of rotational instability due to rupture of the anterior cruciate ligament in an elderly patient
- Fully arthroscopic osteosynthesis with button placement in acute anterior glenoid fracture: a case report
- Arthroscopic visualization of the popliteal hiatus and localization of an intraarticular free body
Más en PUBMED
Más en Google Scholar


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.