Learning curve in the arthroscopic Latarjet technique
Curva de aprendizaje en la técnica de Latarjet artroscópica
Resumen:
Objetivo: analizar los resultados clínicos y radiológicos de la técnica de Latarjet artroscópica evaluando cuantitativamente la curva de aprendizaje.
Material y método: se realizó un estudio prospectivo de los 60 primeros casos intervenidos por un único cirujano principal mediante la técnica de Latarjet artroscópica con un seguimiento mínimo de 24 meses analizando variables subjetivas (escala visual analógica –EVA–) y objetivas (epidemiológicas, radiológicas y complicaciones).
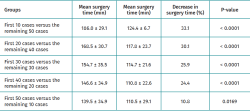
Resultados: se incluyeron 56 varones y 4 mujeres con una edad media de 27,3 años. El tiempo medio de cirugía disminuyó a lo largo de la curva de aprendizaje (p < 0,05); la disminución más importante fue al comparar los 10 primeros casos y los 50 restantes (27,9%). En el 90% de los casos la posición del injerto fue buena o excelente. El 6,66% de los injertos coracoideos se rompieron y el 3,33% de los pacientes presentaron parestesias transitorias del nervio radial y musculocutáneo. Media de la escala de Rowe preoperatoria 42,4 vs. 87,3 en el postoperatorio (p < 0,001).
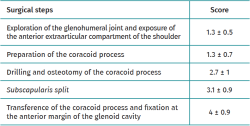
Conclusiones: la experiencia del cirujano afecta significativamente en la duración de la cirugía. La apertura del subescapular, la osteotomía de la coracoides y la transferencia y la fijación de esta son los pasos más complejos. Se ha observado que los resultados clínicos, tras la curva de aprendizaje, son satisfactorios y reproducibles.
Abstract:
Objective: To analyze the clinical and radiological results obtained using the arthroscopic Latarjet technique, with a quantitative assessment of the learning curve.
Material and methods: A prospective study was made of the first 60 cases operated upon by a single main surgeon using the arthroscopic Latarjet technique, with a minimum follow-up of 24 months, analyzing subjective (visual analogue scale [VAS]) and objective variables (epidemiological, radiological and complications).
Results: A total of 56 males and four females, with a mean age of 27.3 years, were included. The mean surgery time decreased over the learning curve (p < 0.05), with the most important decrease corresponding to comparison of the first 10 cases versus the remaining 50 cases (27.9%). In 90% of the cases graft positioning was good or excellent. A total of 6.66% of the coracoid grafts suffered disruption, and 3.33% of the patients presented transient paresthesias of the radial and musculocutaneous nerves. The mean preoperative Rowe score was 42.4 versus 87.3 postoperatively (p < 0.001).
Conclusions: Surgeon experience significantly affects the duration of surgery. Subscapular opening, coracoid osteotomy and transference and fixation are the most complex steps. The clinical outcomes following completion of the learning curve are satisfactory and reproducible.
Introduction
Anterior shoulder instability is common, particularly in young individuals and athletes with high functional demands(1). The most frequent arthroscopic technique for the management of this disorder is Bankart surgery, which has shown very high success rates in most patients(2). Nevertheless, some studies report failure and recurrent dislocation rates of between 20-67%, with failure of this technique being higher among athletes involved in contact sports(3,4).
In the context of instability, some investigators report that bone loss in the anteroinferior part of the glenoid cavity can be seen in 41% of the cases after the first episode; this figure can reach 86% in recurrent glenohumeral instability, with the bone deficit being less than 10% in most of the cases(5). The bone deficit, along with other factors such as an early age at first dislocation, numerous glenohumeral dislocations(6), ligament hyperlaxity and the practice of contact sports, have caused the outcomes to be less satisfactory, with a higher postoperative failure rate(7,8).
The Latarjet technique, first described in 1954, consists of transferring the coracoid process to the anteroinferior part of the glenoid cavity, and has demonstrated good clinical and biomechanical outcomes in the treatment of anterior glenohumeral instability(9). The main advantages of this technique are reconstruction of the bone loss and, in some cases, an increase in the anteroposterior diameter of the glenoid cavity to facilitate glenohumeral congruence, with reinforcement of the anterior capsule by means of the joint tendon and the lower portion of the subscapularis, creating a "hammock effect"(10,11,12).
Some of the complications described with Latarjet surgery are non-consolidation of the coracoid process and the presence of neurological injuries (brachial plexus, axillary nerve, musculocutaneous)(13,14).
In 2007, Lafosse first described the Latarjet technique performed via arthroscopy. Since then, specific instruments have been developed, along with new methods for fixation of the coracoid process(15). The arthroscopic technique results in less postoperative pain during the first two weeks(16), and allows faster recovery than in open surgery, with direct visualization of the glenoid cavity, thereby facilitating the diagnosis of possible concomitant glenohumeral lesions and correct positioning of the coracoid process(15,17).
Despite the studies reporting excellent clinical outcomes, the arthroscopic technique implies longer surgery times(16), is technically complex, and has a complications rate that can reach 11% at two years.
In processes of this kind, a correct surgeon learning curve is crucial in order to obtain good results with the fewest complications possible. The present study analyzes the clinical and radiological results obtained using the arthroscopic Latarjet technique, with an assessment of the learning curve.
Material and methods
A prospective study was made of the first 60 cases operated upon by a single main surgeon using the arthroscopic Latarjet technique, with a minimum follow-up of 24 months.
The study included 60 patients over 18 years of age with recurrent glenohumeral instability and 10% bone loss at anteroinferior level of the glenoid cavity, with off-track Hill-Sachs lesions. Patients with a history of previous bone stop surgery were excluded.
All patients were operated upon according to the technique described by Lafosse(15). The surgical procedure was divided into 5 steps:
- Exploration of the glenohumeral joint and exposure of the anterior extraarticular compartment of the shoulder.
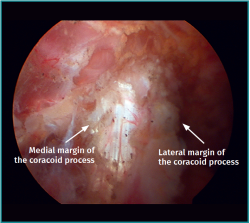
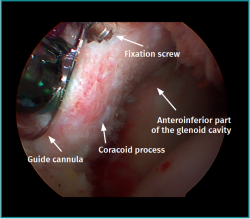
- Preparation of the coracoid process (Figure 1).
- Drilling and osteotomy of the coracoid process.
- Horizontal opening of the subscapularis.
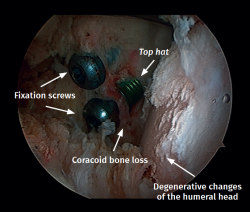
- Transference of the coracoid process and fixation at the anterior margin of the glenoid cavity using cannulated screws (Figure 2).
Subjective (surgeon comfort in performing surgery, visual analogue scale [VAS]) and objective variables (epidemiology, radiology, mean surgery time and complications) were analyzed.
Epidemiological variables
Patient gender and age at the time of surgery were evaluated, along with involvement of the dominant extremity and the practice of contact sports.
Radiological variables
The radiological variables comprised plain radiographs, joint magnetic resonance imaging (arthro-MRI) or conventional MRI, and computed tomography (CT). We assessed bone loss of the anteroinferior portion of the glenoid cavity, the size of the Hill-Sachs lesion and glenoid track.
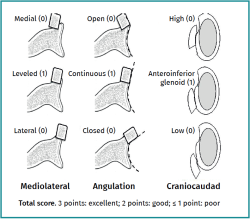
The final position of the graft was measured from the axial and sagittal CT scans performed in the postoperative period at 6 weeks, and at 6 and 12 months, and was considered to be optimum when the graft in the sagittal plane was located at the lower portion of the glenoid cavity, well supported on the anteroinferior wall and in continuity with the surface of the glenoid cavity in the axial plane. Positioning too far lateral may result in the development of early glenohumeral osteoarthrosis, and positioning too far medial might cause surgery to be ineffective.
The score was considered to be either 1 (satisfactory) or 0 (not satisfactory) in each of the planes, based on the position of the graft in relation to the glenoid cavity in the mediolateral and craniocaudad planes, and the angle of the bone stop with respect to the glenoid surface in the axial plane was assessed. The final position was recorded as poor (0-1 points), good (2 points) or excellent (3 points) based on the sum of the scores of the position of the graft in each of the planes (Figure 3).
Clinical and functional variables
The Rowe scale was used to evaluate range of motion (abduction, antepulsion, external and internal rotation), with stability assessing the limitation of patient function.
Mean surgery time
The surgery time was measured in minutes from creation of the first portal to complete closure of all the surgical wounds. Neither the anesthesia time nor the patient positioning time were taken into account. A plot with the mean surgery time in each case was obtained, and a logarithmic trend curve representing the learning curve was calculated, comparing four groups:
- The first 10 cases versus the remaining 50 cases.
- The first 20 cases versus the remaining 40 cases.
- The first 30 cases versus the remaining 30 cases.
- The first 40 cases versus the remaining 20 cases.
- The first 40 cases versus the remaining 10 cases.
Position of the coracoid process
The graft was not considered to be correctly positioned if there was a step of over 3 mm (mm) between the coracoid process and the anterior margin of the glenoid cavity.
Complications
We evaluated the recurrence of instability (episodes of dislocation or glenohumeral dislocation), infection, neurological lesions, reabsorption, osteolysis or a lack of graft consolidation, as well as the presence of glenohumeral osteoarthrosis.
Subjective variables
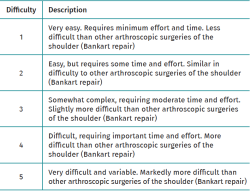
Surgeon comfort in performing the Latarjet arthroscopic procedure was assessed by viewing the videos of each operation, and the degree of difficulty was evaluated by scoring each of the steps from 1 to 5 based on a numerical scale and comparing the difficulty versus that of conventional Bankart repair (Table 1).
Patient satisfaction after surgery was evaluated by means of a VAS from 1 (totally unsatisfied) to 10 (totally satisfied).
The statistical analysis was performed with the online EasyMedStat (version 3.21) application. Evaluation and comparison of the variables was made with the Shapiro-Wilk test, considering an alpha risk of 5% (α = 0.05), and using the Wilcoxon rank sign test. The means of parametric variables were compared with the two-sample Student t-test, with 95% confidence intervals. A comparison was made of the difficulty scores obtained for the 5 steps of the surgical procedure using the Friedman test, with paired comparison of the 5 steps being carried out with the Wilcoxon test. Statistical significance was considered for p < 0.05.
Results
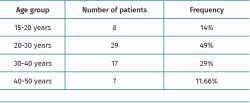
The study sample consisted of 56 males and four females, with a mean age of 27.5 ± 7.8 years (range 15-47), and differences in frequency according to age groups, as can be seen in Table 2.
In 58.3% of the cases the right shoulder was affected, versus the left shoulder in 41.7% of the patients; of note is the fact that the dominant extremity was affected in 53.3% of the cases.
Sixty percent of the patients (n=36) had office jobs, while 40% (n=24) had professions involving sports activities or the lifting of weights above head level.
On examining the sports activities, 3.3% of the patients (n=2) practiced contact sports on a professional level, 42.4% (n=25) were frequently involved in contact sports, and 54.3% (n=33) did not perform sports activities or did so only occasionally.
Arthroscopic Latarjet was performed as primary surgery in 42 patients (n=70%), while in 30% of the cases it was chosen as revision surgery after arthroscopic Bankart surgery associated to remplissage in two individuals.
On the other hand, 76.6% of the patients underwent preoperative study with arthro-MRI, 21.6% with conventional MRI, and 2% with arthroscopic CT. In turn, 32.6% of the patients subjected to arthro-MRI were evaluated with three-dimensional CT, evidencing off-track lesions in the entire sample.
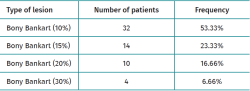
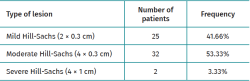
The preoperative radiological findings are shown in Tables 3 and 4(18).
The mean surgery time decreased significantly over the learning curve (p < 0.05). The most important decrease in surgery time (27.9%) was observed on comparing the time between first 10 cases versus the remaining 50 cases (Table 5). The surgeon impressions in the different stages are reported in Table 6, evidencing greater difficulty in subscapularis aperture, osteotomy of the coracoid process, and in its transference and fixation at the anteroinferior part of the glenoid cavity.
The mean revision surgery time was 141.8 ± 5 minutes versus 132.5 ± 7 minutes in the case of the primary stabilizations, though the difference was not statistically significant.
The graft position was excellent in 71.7% of the cases, good in 18.3% and poor in 6.7%, as assessed by the postoperative CT study. Positioning of the graft at the lower part of the glenoid cavity was observed in 99.3% of the cases, though it extended beyond the lower part of the cavity in 3.3% of the cases (n=2) and was found to be too medial in another 3.3% and too lateral in 10% (n=6).
During surgery, four of the coracoid grafts (6.7%) ruptured in part and had to be fixed only with a screw. In addition, two graft avulsions were recorded during the postoperative period - one of them secondary to trauma.
Mild to moderate glenohumeral osteoarthrosis was observed in 30% of the patients during follow-up (Figure 4).
Recurrence of instability was recorded in four patients (6.7%), with the need for revision surgery. Neurological problems in the immediate postoperative period were documented in two patients - transient paresis of the radial nerve in one case and of the musculocutaneous nerve in the other - and resolved without sequelae.
The mean Rowe score improved from 42.4 in the preoperative period to 87.3 in the postoperative period (p < 0.001). The mean external rotation (ER) deficit at 90º was 8.93 ± 7.42º, and the mean ER deficit at 0º was 9.92 ± 8.95º, with the observation of similar values.
Patient satisfaction as assessed by the VAS was 8.75 ± 1.2 on average.
Discussion
The arthroscopic Latarjet procedure is technically very demanding, particularly in some of the phases of the technique such as horizontal subscapularis aperture and the preparation, transference and fixation of the coracoid process at the anteroinferior part of the glenoid cavity.
In our study, and in coincidence with the literature, the most significant difference was the surgery time, which for both the open technique and the arthroscopic procedure was seen to decrease on advancing through the learning curve(19).
It is difficult to compare our surgery times with those of other studies, due to the lack of clear specifications of how time is counted (whether anesthetic preparation is included or not)(19). This study shows a learning curve with a significant decrease in surgery time particularly from the first 10 cases. The decrease even continues after the first 50 cases, evidencing that the learning curve is long(20).
Lafosse et al. also highlighted the complexity of this technique and the importance of the learning curve, observing a significant decrease in surgery time on comparing the first 5 cases versus the times recorded from the first 20 patients (123.8 versus 92.6 min)(21). This study also reflected the difference in times between surgeons, all of them with extensive experience in complex shoulder surgery, indicating that part of the learning curve is dependent on each individual. In addition, that fact of whether the operation constituted primary surgery or revision surgery also exerted an influence(21).
Castricini et al. divided the technique into 5 phases, in the same way as in our study, though some of the phases were placed in a different order. The phases were described as the evaluation and exposure of the glenohumeral joint, subscapularis split, preparation of the coracoid process, and transference and fixation of the graft at the anteroinferior part of the glenoid cavity. Surgery time decreased in all the phases, except in transference of the coracoid process, and conversion to open surgery was seen to be more common at the start of the learning process(22).
In our study there were no conversions to open surgery, and the total surgery time was evaluated without counting the minutes used in each phase.
Coracoid fracture was observed in four patients, in which modification of the usual fixation system proved necessary. Some studies indicate that if there are intraoperative problems in preparing the coracoid process and good fixation cannot be obtained with two screws, other fixation options should be considered, such as the double-button device, in order to avoid surgical failure(23,24). Prior to surgery, it is of interest to assess the size of the coracoid process in order to determine whether there is enough space for positioning both screws.
Positioning of the graft in the sagittal plane remains subject to controversy. Some authors recommend placing it below the 3 o'clock position, while others consider positioning between the 2 and 5 o'clock position to be ideal(11,25). In our study the graft was positioned in the lower quadrant below the 3 o'clock position in 99.3% of the cases. This percentage is far higher than in other studies that only place 57.2% of the grafts in this position, versus 83.4% placed between the 2 and 5 o'clock position(23). This indicates that despite direct vision of the joint, we must be meticulous in releasing the soft tissues in order to position the graft as low as possible and thus avoid recurrence. Our findings are in contradiction to those of some studies that consider that the arthroscopic technique has not significantly improved correct positioning of the coracoid process(26).
Patient satisfaction was high. However, despite the good clinical results and the low percentage of complications, the recurrence rate in our study was higher than described elsewhere in the literature(27). This high recurrence rate may be due to the fact that the bone stop technique was used in the more complex cases with larger bone defects or in revision surgeries.
The coracoid transpositioning techniques are based on a non-anatomical reconstruction of the shoulder that is not free of risks, such as neurovascular damage, subscapularis alterations and an increased presence of glenohumeral osteoarthrosis.
Although in our study there were only two transient injuries of the radial nerve and the musculocutaneous nerve, anatomical studies have evidenced variability in the trajectory of both of these nerves, which increases the risk of nerve damage during this procedure(27). In addition, the fact that the two screws were placed divergent by more than 10º increases the risk of suprascapular nerve damage, particularly attributable to the upper screw(28).
In our series we documented a mean loss of external rotation of 9º, which is slightly lower than reported in the literature, with a 15% loss of total ER(29). This may be due to the position of the bone stop, and to the creation of a scar following the radiofrequency subscapularis split in the arthroscopic technique(23).
The presence of radiological degenerative changes is seen in 30% of the patients following the Latarjet procedure, and is related to a history of recurrent dislocations, prominent implants and lateralization of the coracoid process(30). However, the presence of secondary osteoarthrosis in the radiological studies is not predictive of patient functional loss. In our series increased lateralization of the graft was noted in 10% of the cases, though a long term study would be needed to assess the influence of this circumstance upon the appearance of glenohumeral osteoarthrosis.
The main limitation of the present study is subjective bias in establishing the difficulty of the different surgical steps, since it was carried out retrospectively by observing the surgical videos.
Conclusions
Surgeon experience in performing arthroscopic bone stop techniques significantly affects the duration of surgery. Subscapular opening, coracoid osteotomy and transference and fixation are the most complex steps. Despite the difficulty, the clinical outcomes following completion of the learning curve are satisfactory and reproducible.
Figuras
Figure 2. Transference of the coracoid process and fixation at the anterior margin of the glenoid cavity using cannulated screws. View from portal J.
Figure 3. Scoring system for evaluating the position of the graft following the arthroscopic Latarjet technique.
Tablas
Table 2. Age frequency distribution of the patients subjected to the arthroscopic Latarjet technique
Table 3. Bone defect of the anteroinferior part of the glenoid cavity in preoperative radiological evaluations
Table 4. Size of the Hill-Sachs lesion in the preoperative radiological evaluations according to the classification of Rowe et al.(18)
Información del artículo
Cita bibliográfica
Autores
María Brotat Rodríguez
Unidad de Hombro y Codo. Hospital Universitario Infanta Elena. Valdemoro, Madrid
Servicio de Cirugía Ortopédica y Traumatología. HU Infanta Elena. Valdemoro. Madrid
Diana Morcillo Barrenechea
Servicio de Cirugía Ortopédica y Traumatología. HU Fundación Jiménez Díaz. Universidad Autónoma. Madrid
Rodrigo Antón Mateo
Unidad de Hombro y Codo. Hospital Universitario Infanta Elena. Valdemoro, Madrid
Servicio Cirugía Ortopédica y Traumatología. Hospital Universitario Infanta Elena. Valdemoro. Madrid
Emilio Calvo Crespo
Unidad de Cirugía del Hombro y del Codo. Servicio de Cirugía Ortopédica y Traumatología. Instituto de Investigación Fundación Jiménez Díaz-Capio. Madrid
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Dauzère F, Faraud A, Lebon J, Faruch M, Mansat P, Bonnevialle N. Is the Latarjet procedure risky? Analysis of complications and learning curve. Knee Surg Sports Traumatol Arthrosc. 2016 Feb;24(2):557-63.
-
2Mohtadi NG, Bitar IJ, Sasyniuk TM, Hollinshead RM, Harper WP. Arthroscopic versus open repair for traumatic anterior shoulder instability: a meta-analysis. Arthroscopy. 2005 Jun;21(6):652-8.
-
3Joshi MA, Young AA, Balestro JC, Walch G. The Latarjet-Patte procedure for recurrent anterior shoulder instability in contact athletes. Clin Sports Med. 2013 Oct;32(4):731-9.
-
4Cho NS, Hwang JC, Rhee YG. Arthroscopic stabilization in anterior shoulder instability: collision athletes versus noncollision athletes. Arthroscopy. 2006 Sep;22(9):947-53.
-
5Griffith JF, Antonio GE, Yung PS, et al. Prevalence, pattern, and spectrum of glenoid bone loss in anterior shoulder dislocation: CT analysis of 218 patients. AJR Am J Roentgenol. 2008 May;190(5):1247-54.
-
6Randelli P, Ragone V, Carminati S, Cabitza P. Risk factors for recurrence after Bankart repair a systematic review. Knee Surg Sports Traumatol Arthrosc. 2012 Nov;20(11):2129-38.
-
7Calvo E, Granizo JJ, Fernández-Yruegas D. Criteria for arthroscopic treatment of anterior instability of the shoulder: a prospective study. J Bone Joint Surg Br. 2005 May;87(5):677-83.
-
8Boileau P, Villalba M, Héry JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006 Aug;88(8):1755-63.
-
9Giles JW, Boons HW, Elkinson I, et al. Does the dynamic sling effect of the Latarjet procedure improve shoulder stability? A biomechanical evaluation. J Shoulder Elbow Surg. 2013 Jun;22(6):821-7.
-
10Longo UG, Loppini M, Rizzello G, Ciuffreda M, Maffulli N, Denaro V. Latarjet, Bristow, and Eden-Hybinette procedures for anterior shoulder dislocation: systematic review and quantitative synthesis of the literature. Arthroscopy. 2014 Sep;30(9):1184-211.
-
11Boileau P, Gendre P, Baba M, et al. A guided surgical approach and novel fixation method for arthroscopic Latarjet. J Shoulder Elbow Surg. 2016 Jan;25(1):78-89.
-
12Bliven KCH, Parr GP. Outcomes of the Latarjet Procedure Compared With Bankart Repair for Recurrent Traumatic Anterior Shoulder Instability. J Athl Train. 2018 Feb;53(2):181-3.
-
13Lafosse L, Boyle S, Gutiérrez-Aramberri M, Shah A, Meller R. Arthroscopic Latarjet procedure. Orthop Clin North Am. 2010 Jul;41(3):393-405.
-
14Gupta A, Delaney R, Petkin K, Lafosse L. Complications of the Latarjet procedure. Curr Rev Musculoskelet Med. 2015 Mar;8(1):59-66.
-
15Lafosse L, Lejeune E, Bouchard A, Kakuda C, Gobezie R, Kochhar T. The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability. Arthroscopy. 2007 Nov;23(11):1242.e1-5.
-
16Horner NS, Moroz PA, Bhullar R, et al. Open versus arthroscopic Latarjet procedures for the treatment of shoulder instability: a systematic review of comparative studies. BMC Musculoskelet Disord. 2018 Jul 25;19(1):255.
-
17Boileau P, Bicknell RT, El Fegoun AB, Chuinard C. Arthroscopic Bristow procedure for anterior instability in shoulders with a stretched or deficient capsule: the "belt-and-suspenders" operative technique and preliminary results. Arthroscopy. 2007 Jun;23(6):593-601.
-
18Rowe CR, Zarins B, Ciullo JV. Recurrent anterior dislocation of the shoulder after surgical repair. Apparent causes of failure and treatment. J Bone Joint Surg Am. 1984 Feb;66(2):159-68.
-
19Ekhtiari S, Horner NS, Bedi A, Ayeni OR, Khan M. The Learning Curve for the Latarjet Procedure: A Systematic Review. Orthop J Sports Med. 2018 Jul 26;6(7):2325967118786930.
-
20Cunningham G, Benchouk S, Kherad O, Lädermann A. Comparison of arthroscopic and open Latarjet with a learning curve analysis. Knee Surg Sports Traumatol Arthrosc. 2016 Feb;24(2):540-5.
-
21Leuzinger J, Brzoska R, Métais P, et al. Learning Curves in the Arthroscopic Latarjet Procedure: A Multicenter Analysis of the First 25 Cases of 5 International Surgeons. Arthroscopy. 2019 Aug;35(8):2304-11.
-
22Castricini R, De Benedetto M, Orlando N, Rocchi M, Zini R, Pirani P. Arthroscopic Latarjet procedure: analysis of the learning curve. Musculoskelet Surg. 2013 Jun;97 Suppl 1:93-8.
-
23Kordasiewicz B, Małachowski K, Kiciński M, et al. Intraoperative graft-related complications are a risk factor for recurrence in arthroscopic Latarjet stabilisation. Knee Surg Sports Traumatol Arthrosc. 2019 Oct;27(10):3230-9.
-
24Bonnevialle N, Thélu CE, Bouju Y, et al. Arthroscopic Latarjet procedure with double-button fixation: short-term complications and learning curve analysis. J Shoulder Elbow Surg. 2018 Jun;27(6):e189-e195.
-
25Kany J, Flamand O, Grimberg J, et al. Arthroscopic Latarjet procedure: is optimal positioning of the bone block and screws possible? A prospective computed tomography scan analysis. J Shoulder Elbow Surg. 2016 Jan;25(1):69-77.
-
26Wellmann M, Petersen W, Zantop T, et al. Open shoulder repair of osseous glenoid defects: biomechanical effectiveness of the Latarjet procedure versus a contoured structural bone graft. Am J Sports Med. 2009 Jan;37(1):87-94.
-
27Freehill MT, Srikumaran U, Archer KR, McFarland EG, Petersen SA. The Latarjet coracoid process transfer procedure: alterations in the neurovascular structures. J Shoulder Elbow Surg. 2013 May;22(5):695-700.
-
28Lädermann A, Denard PJ, Burkhart SS. Injury of the suprascapular nerve during latarjet procedure: an anatomic study. Arthroscopy. 2012 Mar;28(3):316-21.
-
29Lafosse L, Boyle S. Arthroscopic Latarjet procedure. J Shoulder Elbow Surg. 2010 Mar;19(2 Suppl):2-12.
-
30Waterman BR, Kilcoyne KG, Parada SA, Eichinger JK. Prevention and management of post-instability glenohumeral arthropathy. World J Orthop. 2017 Mar 18;8(3):229-41.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- The COVID hangover
- Results of the arthroscopic treatment of acute bony Bankart lesion using the original Porcellini-Sugaya technique and the double-row modified procedure
- Assessment of tibial translation in experimental models of anterior cruciate ligament reconstructions: is dual tibial fixation indicated?
- Learning curve in the arthroscopic Latarjet technique
- Clinical outcomes of the anteromedial technique versus the transtibial technique in reconstruction of the anterior cruciate ligament: a systematic review and meta-analysis of randomized clinical trials
- Basic sciences in reconstruction of the anterior cruciate ligament with the ischiotibial tendons (a narrative review)
- Arthroscopic hip surgery in femoroacetabular impingement
- Circumferential 270º reconstruction of the hip labrum through arthroscopy with knotless tensionable technology Surgical technique
- Arthroscopic capsule reconstruction with dermal mesh plus segmental labral reconstruction with tibialis anterior allograft in recurrent postsurgical hip microinstability
- Synthetic polyethylene mesh augmentation for chronic patellar tendon rupture repair
- The Giant’s Causeway “inside the shoulder”
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.