Arthroscopic capsule reconstruction with dermal mesh plus segmental labral reconstruction with tibialis anterior allograft in recurrent postsurgical hip microinstability
Reconstrucción capsular artroscópica con malla dermal más reconstrucción labral segmentaria con tibial anterior en microinestabilidad recurrente de cadera posquirúrgica
Resumen:
La cápsula es uno de los principales estabilizadores estáticos de la articulación de la cadera, junto con el labrum y el ligamento redondo. Una capsulotomía irreparable con un defecto en ella secundario a una artroscopia de cadera tiene implicación como causa potencial de resultados inferiores, dolor posquirúrgico, daño condral y artroscopias de revisión. Un procedimiento de reconstrucción capsular en estos casos puede reparar el defecto anatómico y mejorar la función biomecánica de la articulación. La reconstrucción labral circunferencial se realiza cuando existe un desgarro labral extenso, una calidad de tejido pobre o un labrum pequeño o atrófico. La reconstrucción segmentaria está indicada si el defecto es limitado y existe una unión condrolabral alterada. El objetivo de esta publicación es presentar la técnica quirúrgica y los resultados iniciales de un caso de reconstrucción simultánea del labrum acetabular con aloinjerto de tibial anterior segmentaria y de cápsula articular con malla dermal acelular en un caso de inestabilidad de cadera posquirúrgica por deficiencia mixta labral y capsular en una mujer de 38 años de edad con antecedente de cirugía previa por choque femoroacetabular derecho que consultaba por presentar dolor residual y sensación de falta de estabilidad y que presentaba en la artrorresonancia áreas de degeneración/rerrotura condrolabral acetabular y una cápsula articular deficiente sin alteraciones estructurales de versión en acetábulo y fémur, con gran desplazamiento a la distracción articular mediante tracción blanda. Esta combinación técnica no ha sido publicada previamente. Se enumeran ventajas y limitaciones del procedimiento, y los puntos clave que se deben tener en cuenta.
Abstract:
The capsule is one of the main static stabilizers of the hip joint, together with the labrum and the round ligament. A non-repairable capsulotomy involving a defect secondary to hip arthroscopy is a potential cause of poorer outcomes, postsurgical pain, chondral damage and revision arthroscopies. In these case, a capsule reconstruction procedure may repair the anatomical defect and improve the biomechanical function of the joint. Circumferential labral reconstruction is carried out in cases characterized by extensive labral tearing, poor tissue quality, or a small or atrophic labrum. Segmental reconstruction in turn is indicated in cases characterized by a limited defect size and the existence of an altered chondrolabral junction. The present study describes the surgical technique and the early outcomes of a case of simultaneous reconstruction of the acetabular labrum with segmental anterior tibial and joint capsule allograft plus an acellular dermal mesh in a case of postoperative hip instability due to mixed labral and capsular deficiency in a 38-year-old woman with a history of prior surgery because of right femoroacetabular impingement. The patient presented with residual pain and instability sensation. Magnetic resonance imaging evidenced acetabular chondrolabral degeneration / repeat rupture and a deficient joint capsule, without version structural alterations of the acetabulum and femur, and presenting great displacement in response to gentle traction joint distraction. This combined technique has not been previously published. The advantages and limitations of the procedure are commented, along with the key points to be taken into account.
Introduction
With the recent rise in the use of arthroscopy in application to the hip, the revision rates due to inadequate outcomes has increased. The management of these patients with residual pain and recurrent symptoms is a challenge as far as diagnosis and treatment are concerned. Although the most common causes of failure after hip arthroscopy include incomplete resection of the cam deformity, a scantly reported complication is excessive resection of the capsule, which results in loss of joint sealing. A non-repairable capsulotomy, or postsurgical capsule rupture with a capsule defect following arthroscopy, is a potential cause of poorer outcomes, postsurgical pain, chondral damage and revision arthroscopies(1,2).
Arthroscopic capsular reconstruction is a recently published technique that seeks to resolve postsurgical capsule defects. Labral reconstruction using graft material is an increasingly common technique in primary and revision surgery of the hip, involving tissue implantation to also restore joint sealing in cases where repair is not possible. Such reconstruction may be segmental or circumferential (270°). Circumferential labral reconstruction is carried out in cases characterized by extensive labral tearing, poor tissue quality, or a small or atrophic labrum. Segmental reconstruction is indicated in the presence of a limited defect size and the existence of an altered chondrolabral junction(3,4).
The present study describes the surgical technique and the initial outcomes of simultaneous reconstruction of the acetabular labrum with segmental tibialis anterior and joint capsule allograft with the Epiflex® dermal mesh, in a case of postsurgical hip instability. This combination has not been previously published.
Surgical technique
Background and diagnostic tests
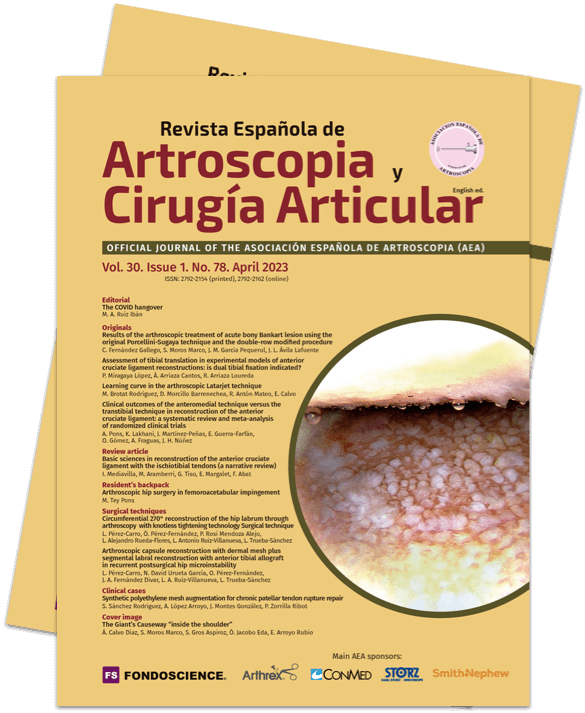
A 38-year-old woman subjected to surgery three years ago due to right femoroacetabular impingement presented with residual pain. At exploration, the Faber and impingement maneuvers were very positive, as was the dial test. Anterior instability maneuvering (abduction and extension) with apprehension during gentle external rotation maneuvers also proved positive. No rotational anomalies were evidenced at exploration. The modified Harris score was 68 points. Radiographically, the head-neck junction was correct, in the same way as acetabular coverage. On the other hand, joint magnetic resonance imaging showed areas of 11-3 o'clock acetabular chondrolabral degeneration / re-rupture and a deficient joint capsule corresponding to type 3 of the Aoki classification(5) (Figure 1), with no version structural alterations of the acetabulum and femur. In addition, important joint distraction displacement with gentle traction was observed. Postsurgical hip microinstability due to mixed capsular and labral joint sealing loss was diagnosed. In view of these findings, simultaneous arthroscopic labral and capsular reconstruction was proposed.
Positioning
Under combined (spinal and general) anaesthesia, the patient is placed on the traction table in supine decubitus with the contralateral leg in abduction. The hip to be operated upon is placed in 10-15º flexion and is moved towards the neutral midline. The hip is distracted through longitudinal traction. The foot of the leg to be operated upon is rotated internally to move the femoral neck parallel to the floor, and the table is inclined 10º towards the opposite side(6). Under conditions of asepsis and antisepsis, the surgical field is prepared, and the anatomical references are marked: anterosuperior iliac spine, trochanter and longitudinal line from the spine to the centre of the patella, which determines the safe zone for working, avoiding the risk of vascular and nerve damage.
reacae.30178.fs2212025-figure2.png

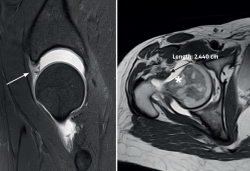
Figure 2. Portals: 1) anterolateral (ALP): upper margin of the greater trochanter in line with its anterior margin or 1 cm anterior and 1 cm superior to the tip of the greater trochanter; 2) middle anterior portal (MAP): 6-7 cm distal to the anterolateral portal, at an angle of about 60-70º; 3) distal anterolateral access (DALA): 3-4 cm distal and 1-2 cm anterior to the ALP; 4) proximal middle anterior portal (PMA): 2-3 cm proximal and 2-3 cm posterior to the MAP; 5) accessory DALA: 2-3 cm anterior to the standard DALA; 6) posterolateral portal (PLP): upper margin of the greater trochanter in line with its posterior margin or 1 cm posterior and 1 cm superior to the tip of the greater trochanter. The asterisk shows the zone of the greater trochanter.
Portals
The arthroscopic approach is made using the all inside technique, with initial access to the central compartment and maximum capsule preservation. Six arthroscopic portals are used for this procedure: 1) anterolateral (ALP): upper margin of the greater trochanter in line with its anterior margin or 1 cm anterior and 1 cm superior to the tip of the greater trochanter; 2) middle anterior portal (MAP): located 6-7 cm distal to the anterolateral portal, at an angle of about 60-70º; 3) distal anterolateral access (DALA): located 3-4 cm distal and 1-2 cm anterior to the ALP; 4) proximal middle anterior portal (PMA): located 2-3 cm proximal and 2-3 cm posterior to the MAP; 5) accessory DALA: 2-3 cm anterior to the standard DALA; and 6) posterolateral portal: upper margin of the greater trochanter in line with its posterior margin or 1 cm posterior and 1 cm superior to the tip of the greater trochanter (Figure 2).
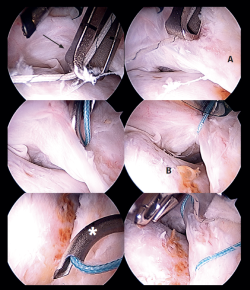
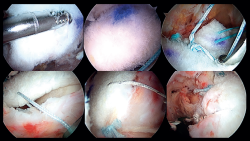
Arthroscopy, labral check, preparation or the acetabulum and of the capsule zone
Once the anterolateral and modified anterior portals have been established, an interportal capsulotomy is performed to allow handling of the instruments within the joint. The vision portal during most of the surgery is the anterolateral portal. During the procedure a degenerated labrum is observed, with re-ruptures, adherences and an impaired chondrolabral junction. In addition, an important anterior capsule defect is observed. This combination clearly determines the loss of joint sealing (Figure 3). In a first step we remove the deficient labrum in the anterosuperior zone and the acetabular margin is gently refreshed with a 4.0 mm round bur (Stryker®) to expose the proximal anatomical insertion of the iliofemoral ligament: from the upper part of the iliopsoas recess (approximately in the 2:30 o'clock position) to the anteroinferior portion of the anteroinferior iliac spine (AIIS) (approximately in the 12 o'clock position). The remaining capsule tissue in the zona orbicularis(ZO) is refreshed with a synoviotome in preparation for the distal anastomosis. Then, the hip is examined through flexion and rotation to evaluate the capsule defect in these positions. Through the DALA we place two 2.1 mm PressFT® (Conmed) suture anchorings loaded with Hi-Fi number 2 suture in the acetabular margin proximal to the labrum, in the insertion zone of the iliofemoral ligament, at the 12 and 2:30 o'clock positions, and the sutures are exteriorized through the proximal middle anterior portal (PMA) (Figure 4). These sutures will be used for the acetabular or proximal insertion of the capsule dermal graft.
reacae.30178.fs2212025-figure4.png

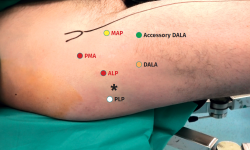
Figure 4. Right hip. Arthroscopic view of the placement of the anchorings: needle, dilator and paddle through the proximal middle anterior portal (PMA) for posterior extraction of the sutures of the proximal anchorings. A: acetabulum; X: proximal anchorings for fixation of the dermal mesh; Y: distal anchorings for fixation of the tibialis anterior tendon. View from the anterolateral port.
Preparation of the segmental acetabular reconstruction
For the treatment of the labrum we perform labral reconstruction with tibialis anterior allograft using the pull through technique(7) and tensionable technology, employing the posterolateral portal as accessory portal for positioning the graft. For this procedure, use is made of a tibialis anterior allograft that is prepared to obtain a diameter of 6-7 mm and a length of about 18 cm. Using FiberLoop® suture, the extremities are prepared with the SpeedWhip® (Arthrex) technique (Figure 5). Once the graft has been prepared, four 1.8 mm FiberTak® Knotless anchorings with tensionable technology (Arthrex) are implanted in the acetabular margin in the 11 to 3 o'clock position, distal to the previously mentioned anchorings, which we will refer to as second row anchorings, through the middle anterior portal or from the DALA, and then we retrieve the sutures of these anchorings through the DALA. During perforation and pre-drilling of the anchoring, the arthroscope is to be placed in a position allowing assessment of the joint cartilage, in order to make sure that the drill is not located between the subchondral bone and the surface of the joint cartilage. In order to prevent the anchorings from penetrating into the acetabular cartilage, the angle of the margin must be determined to ensure adequate placement. The successive filaments are placed in the field aligned and spread out in a fan-like manner from inferior-anterior to posterior-superior.
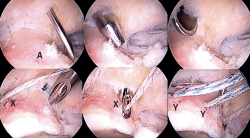
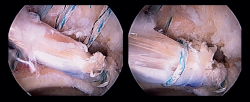
Introduction of the graft for labral reconstruction
Once all the sutures have been positioned, forceps are introduced from the posterolateral portal, taking care that they lie posterior to the last anchoring, with positioning within the joint. From the middle anterior portal we introduce the suture anchored to what will be the posterior part of the graft, likewise taking care that it lies anterior to the most anterior anchoring. This suture is retrieved from the posterolateral portal using the previously introduced forceps, applying traction to introduce the graft, and making it emerge through the posterolateral portal (Figure 6). At this point we fix the graft by passing sutures from the most anterior anchoring of the second row of anchorings, through the anterior part of the tibialis tendon, and it is then finally introduced and sutured. The sutures are then passed around the tendon graft in sequence, and are tightened little by little, maintaining traction from the posterolateral portal, and fixing and positioning the entire plasty from anterior to posterior (Figure 7). Once all these steps have been completed, the excess graft is radiofrequency amputated from the posterolateral portal.
reacae.30178.fs2212025-figure6.png

Figure 6. External view: tibialis anterior tendon (arrow) prepared for insertion in the joint through traction from the posterior portal, sutures in the proximal middle anterior portal (PMA) for proximal capsular anchoring (triangle), tensionable sutures in DALA for labral reconstruction (asterisk).
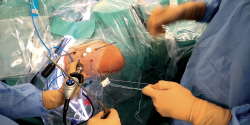
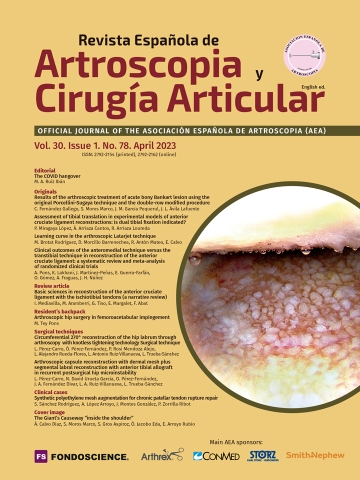
Capsular reconstruction procedure
Treatment of the capsule defect is carried out through capsular reconstruction using the modified kite technique described by Ellman(8). To perform this technique, we measure the dimensions of the proximal-distal capsule defect using the shoulder capsular reconstruction guide (Arthrex). It is important to measure the capsule defect in extension in order to avoid discordances. The last step in the preparation phase is to place two distal simple sutures in the native capsule using a SlingShot® (Stryker) suture passing device, and which will serve as a guide for the definitive sutures (Figure 8). The distal anterior suture is passed and reserved through the accessory DALA, and the distal posterior suture is passed and reserved through the DALA. Lastly, we prepare and cut an acellular dermal graft (Epiflex®) suited to the dimensions of the graft (in this case 2 x 2 cm). One of the extremities of the sutures of the anchorings previously placed at acetabular level and reserved in the proximal middle anterior portal (PMA) is extracted through the DALA and is passed through the proximal portion of the graft using Scorpion® (Arthrex) forceps. In the distal portion of the graft we also introduce FiberWire® number 2 sutures using Scorpion® forceps (Figure 9). Once the graft has been prepared, it is placed inside the joint and fixed at proximal level (Figure 10). Fixation of the distal portion of the capsule is then carried out. The point of this distal fixation is a soft tissue-to-soft tissue anastomosis in the zona orbicularis, which often marks the distal extent of the capsule defect according to most of the capsulectomy procedures. For this purpose we use the stitches previously placed and reserved in the accessory DALA and the DALA as a shuttle. Medial and lateral fixation to the capsule remains is then performed with FiberWire® number 2 stitches (Figure 11). The sutures are knotted with the hip in 10º flexion and neutral rotation. Finally, we check the stability of the graft through flexion and rotation movements. An illustration of the final result of the capsular reconstruction procedure and of the segmental labral reconstruction is shown (Figure 12).
reacae.30178.fs2212025-figure8.png

Figure 8. Arthroscopic views: measurement of the capsule defect with the shoulder capsular reconstruction guide (Arthrex) (black arrow) and guide sutures for distal fixation in remnant capsule (A) using a SlingShot® (Stryker) suture passing device (white star). Head-neck transition zone (B). View from the anterolateral port.
Postoperative rehabilitation
The patient is discharged the day after surgery and follows the usual postoperative rehabilitation for labral repair and decompression due to femoroacetabular impingement, with weight bearing assisted by crutches and circumduction movements and static bicycling during 6 weeks. The patient is to avoid abduction in excess of 20º and extension, and flexion is to be limited to 80-90º and external rotation to 20º during two months. Then, usual rehabilitation for the recovery of mobility and strength is indicated, with progressive conditioning. Physical activity begins after three months, and after about 6 months a gradual return to sports activity is allowed. In the present case, the patient experienced important improvement of her microinstability and inguinal symptoms, with a modified Harris score of 86 points, and continues with periodic controls to assess her long-term evolution.
Discussion
The present study describes a case of postsurgical hip microinstability secondary to mixed labral and capsular deficiency following previous surgery, and with no version structural alterations of the acetabulum and femur. Recently, specific techniques have been developed in hip arthroscopy that are usually only used in revision scenarios such as labral reconstruction and capsular reconstruction. The capsule is one of the main static stabilizers of the hip joint, together with the labrum and the round ligament(9). In arthroscopy of the hip, capsulotomy is routinely performed in most centers to secure better instrument visualization and handling. In this respect, a balance has been sought between adequate visualization and minimum damage to the native structures. The two most common types of capsulotomy are the interportal capsulotomy and the short or long T capsulotomy, in which the integrity of the iliofemoral ligament is affected. This ligament is the most important of the three that conform the reinforcing structures of the capsule (iliofemoral, ischiofemoral and pubofemoral), and is moreover located in its weakest zone(9). For this reason, the evolution of hip preservation surgery has led to the development of arthroscopic techniques for repairing the capsule(10). Although there is no consensus regarding capsule repair in patients subjected to hip arthroscopy, clinical and biomechanical studies have demonstrated that arthroscopic capsule repair is probably very beneficial for the patient(9,10,11,12).
With regard to the types of iatrogenic capsule defects following hip arthroscopy, the group of Aoki(5) published a very useful classification for deciding their treatment, based on the joint magnetic resonance imaging findings: grade 0 (normal capsule volume and anatomy); grade 1 (increased capsule volume and redundancy, but with the anterior capsule continuous and intact); grade 2 (intact capsule continuity but with irregular thickness and focal tearing or alterations); and grade 3 (highly irregular capsule contour and important fluid extravasation through the defect). Direct repair techniques usually suffice in grade 1 and 2 defects, though in grade 3 defects the risk of failure following such repair is high; in these situations it is therefore advisable to consider capsular reconstruction techniques(8).
Historically, capsular reconstruction procedures to improve hip biomechanics have involved open surgery through the anterior approach of Smith-Petersen for reconstruction of the iliofemoral ligament(13,14). However, in recent years and thanks to technical improvements in hip arthroscopy, different arthroscopic capsular reconstruction procedures have been published involving the implantation and use of autografts, allografts and synthetic materials(8,15,16,17,18,19). Due to their degree of difficulty, these techniques require a protocol and strategy for introducing the graft, handling the sutures and fixation, in order to make them safe and reproducible. The use of decellularized dermal allografts involves a very low risk of infection transmission compared with fascia lata allografts, without affecting their biomechanical and biochemical properties, and avoids comorbidities and the probability of complications at the donor site posed by autografts. Although technically demanding, capsular reconstruction offers a surgical solution for capsule defects, with good short term outcomes, avoiding episodes of microinstability and improving joint sealing(20). Medium and long term studies will determine the true efficacy of this technique.
Labral reconstruction using graft material is an increasingly common technique in primary and revision surgery of the hip, involving tissue implantation to also restore the joint sealing effect. Such reconstruction may be segmental or circumferential (270°). Circumferential labral reconstruction is carried out in cases characterized by extensive labral tearing, poor tissue quality, or a small or atrophic labrum. Segmental reconstruction in turn is indicated in cases characterised by a limited defect size and the existence of an altered chondrolabral junction. Domb et al. published their knotless pull-through technique for segmental or circumferential acetabular reconstruction, which offered the advantage of obviating precise measurements, since the use of a graft of surplus length implied that the excess graft could be amputated after fixation. The use of a tibialis anterior tendon allograft adds the advantage of avoiding the complications of autografts, and the use of knotless tensionable technology facilitates performance of this complex technique(4,7). Nho et al. have recently published a technical combination similar to that described in this article, performing augmentation or reinforcement instead of labral reconstruction associated to the capsular reconstruction technique(21). Augmentation or reinforcement is indicated when there is preservation of the chondrolabral junction.
In the present case we decided to perform labral reconstruction instead of augmentation or reinforcement, since the chondrolabral junction was affected.
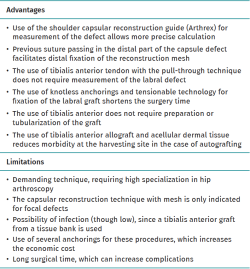
Table 1 describes the advantages and limitations of the procedure, and Table 2 indicates the key points to be taken into account.
Conclusions
Labral reconstruction and capsular reconstruction in a young patient with absence of labral function and with capsule deficit, with recurrent pain after hip arthroscopy, is a surgical option for preserving the physiological integrity of the hip joint. The microinstability symptoms experience notorious improvement in these patients. The technique is complex and must be performed by surgeons with extensive experience in surgeries of this kind. This combined technique has not been previously described.
Supplementary material
The video technique accompanying this article can be seen at:
Figuras
Figure 1. Right hip: joint magnetic resonance imaging view showing labral deficiency and re-ruptures (arrow), and an important capsular defect (star) with marked joint displacement upon traction.
Figure 2. Portals: 1) anterolateral (ALP): upper margin of the greater trochanter in line with its anterior margin or 1 cm anterior and 1 cm superior to the tip of the greater trochanter; 2) middle anterior portal (MAP): 6-7 cm distal to the anterolateral portal, at an angle of about 60-70º; 3) distal anterolateral access (DALA): 3-4 cm distal and 1-2 cm anterior to the ALP; 4) proximal middle anterior portal (PMA): 2-3 cm proximal and 2-3 cm posterior to the MAP; 5) accessory DALA: 2-3 cm anterior to the standard DALA; 6) posterolateral portal (PLP): upper margin of the greater trochanter in line with its posterior margin or 1 cm posterior and 1 cm superior to the tip of the greater trochanter. The asterisk shows the zone of the greater trochanter.
Figure 3. Right hip: arthroscopic view showing the combined labral and capsular deficiency. A: labrum; B: deficient capsule and capsule defect. View from the anterolateral port.
Figure 4. Right hip. Arthroscopic view of the placement of the anchorings: needle, dilator and paddle through the proximal middle anterior portal (PMA) for posterior extraction of the sutures of the proximal anchorings. A: acetabulum; X: proximal anchorings for fixation of the dermal mesh; Y: distal anchorings for fixation of the tibialis anterior tendon. View from the anterolateral port.
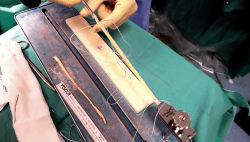
Figure 5. External view of the preparation of the tibialis anterior allograft with FiberLoop® suture and SpeedWhip® technique (Arthrex).
Figure 6. External view: tibialis anterior tendon (arrow) prepared for insertion in the joint through traction from the posterior portal, sutures in the proximal middle anterior portal (PMA) for proximal capsular anchoring (triangle), tensionable sutures in DALA for labral reconstruction (asterisk).
Figure 7. Arthroscopic view of segmental labral reconstruction with tibialis anterior allograft with fixation using knotless tensionable technology. View from the anterolateral port.
Figure 8. Arthroscopic views: measurement of the capsule defect with the shoulder capsular reconstruction guide (Arthrex) (black arrow) and guide sutures for distal fixation in remnant capsule (A) using a SlingShot® (Stryker) suture passing device (white star). Head-neck transition zone (B). View from the anterolateral port.
Figure 10. External view of introduction of the dermal mesh. Bottom right corner: arthroscopic view.
Figure 11. Fixation of the dermal mesh at proximal, distal, medial and lateral level. View from the anterolateral port.
Figure 12. Illustration of the capsular reconstruction procedure (A) and of the segmental labral reconstruction (arrow) (B).
Tablas
Información del artículo
Cita bibliográfica
Autores
Luis Pérez Carro
Servicio de Cirugia Ortopedica y Traumatología. Hospital Clínica Mompía. Santander. Cantabria.
Servicio de Cirugia Ortopedica y Traumatología. Hospital Marqués Valdecilla. Santander
Servicio de Cirugia Ortopedica y Traumatología. Centro Médico Lealtad. Santander
Nicolas David Urueta García
Hospital Mompía. Santander, Cantabria
Óscar Pérez Fernández
Facultad de Medicina Universidad de Cantabria
Hospital Mompía. Santander, Cantabria
Jose Antonio Fernández Divar
Hospital Mompía. Santander, Cantabria
Luis Antonio Ruiz Villanueva
Hospital Mompía. Santander, Cantabria
Lorena Trueba Sánchez
Hospital Mompía. Santander, Cantabria
Cirugía Ortopédica y Traumatología. Hospital Universitario de Burgos
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Domb BG, Stake CE, Finley ZJ, Chen T, Giordano BD. Influence of capsular repair versus unrepaired capsulotomy on 2-year clinical outcomes after arthroscopic hip preservation surgery. Arthroscopy. 2015;31:643-50.
-
2Frank RM, Lee S, Bush-Joseph CA, Kelly BT, Salata MJ, Nho SJ. Improved outcomes after hip arthroscopic surgery in patients under- going T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014;42(11):2634-42.
-
3Pérez-Carro L, Gutiérrez Castanedo G, Menéndez Solana G, Fernandez-Divar JA. Cirugía conservadora de cadera: artroscopia de cadera. En: Combalia Aleu A (coord.). Traumatología y ortopedia. Miembro inferior. Barcelona: GEA Consultoría Editorial, S.L.; 2022. pp. 119-31.
-
4Pérez-Carro L, Mendoza Alejo P, Pérez Fernández O, Rueda Flores LA, Ruiz Villanueva LA, Trueba Sánchez L. Reconstrucción de labrum de cadera circunferencial 270° vía artroscópica con tecnología tensionable sin nudos. Técnica quirúrgica. Rev Esp Artrosc Cir Articul. 2022. En prensa.
-
5O'Neill DC, Mortensen AJ, Cannamela PC, Aoki SK. Clinical and radiographic presentation of capsular iatrogenic hip instability after previous hip arthroscopy. Am J Sports Med. 2020 Oct;48(12):2927-32.
-
6Pérez-Carro L, Galindo C, Estany E, Adrio RG, Golano P, Vega J. Positioning and distraction options. Hip Arthroscopy Indications and Technique. Rome, Italy: Cic Edicione Internationale; 2011. pp. 9-16.
-
7Sabetian PW, Owens JS, Maldonado DR, et al. Circumferential and Segmental Arthroscopic Labral Reconstruction of the Hip Utilizing the Knotless Pull-Through Technique with All-Suture Anchors. Arthrosc Tech. 2021 Sep 8;10(10):e2245-e2251.
-
8Scheidt M, Bhatia S, Fenoglio Z, Ellman MB. Capsular Reconstruction of the Hip Using Modified Kite Technique: A Technical Guide for Efficient Graft Management and Fixation. Arthrosc Tech. 2021 Jan 20;10(1):e209-e216.
-
9Philippon MJ, Michalski MP, Campbell KJ, et al. A quantitative analysis of hip capsular thickness. Knee Surg Sports Traumatol Arthrosc 2015;23:2548-53.
-
10Ortiz-Declet V, Mu B, Chen AW, et al. Should the capsule be repaired or plicated after hip arthroscopy for labral tears associated with femoroacetabular impingement or instability? A systematic review. Arthroscopy. 2018;34: 303-18.
-
11Domb BG, Stake CE, Finley ZJ, Chen T, Giordano BD. Influence of capsular repair versus unrepaired capsulotomy on 2-year clinical outcomes after arthroscopic hip preservation surgery. Arthroscopy. 2015;31:643-50.
-
12Domb BG, Chaharbakhshi EO, Perets I, Walsh JP, Yuen LC, Ashberg LJ. Patient-reported outcomes of capsular repair versus capsulotomy in patients undergoing hip arthroscopy: minimum 5-year follow-up. A matched comparison study. Arthroscopy. 2018;34:853-63.e851.
-
13Kurz AZ, Memon M, Williams D, Ayeni OR. Anterior Capsule Reconstruction of the Native Hip: A Technique Guide. Arthrosc Tech. 2019 Sep 26;8(10):e1247-e1253.
-
14Gehrman M, Cornell M, Seeley M. Iatrogenic Hip Instability After Hip Arthroscopy: Is There a Role for Open Capsular Reconstruction?: A Case Report. JBJS Case Connect. 2019 Apr-Jun;9(2):e0091.
-
15Trindade CA, Sawyer GA, Fukui K, Briggs KK, Philippon MJ. Arthroscopic capsule reconstruction in the hip using iliotibial band allograft. Arthrosc Tech. 2015 Feb 16;4(1):e71-4.
-
16Perets I, Hartigan DE, Walsh JP, Chaharbakhshi E, Close MR, Domb BG. Arthroscopic Capsular Reconstruction of the Hip With Acellular Dermal Extracellular Matrix: Surgical Technique. Arthrosc Tech. 2016 Sep 5;5(5):e1001-e1005.
-
17Byrd JWT. Hip Capsular Reconstruction Made Easy: The Timing and the Technique. Arthrosc Tech. 2020 Dec 19;10(1):e73-e78.
-
18Larson CM, Williams BT, Bessa F, et al. Revision Hip Capsular Repair and Augmentation With a Bioinductive Implant After a Post-arthroscopy Hip Subluxation Event. Arthrosc Tech. 2020 Mar 11;9(4):e453-e458.
-
19Featherall J, Tomasevich KM, O'Neill DC, Mortensen AJ, Aoki SK. Arthroscopic Hip Capsule Reconstruction for Anterior Hip Capsule Insufficiency in the Revision Setting. Arthrosc Tech. 2021 Apr 26;10(5):e1339-e1344.
-
20Philippon MJ, Trindade CAC, Goldsmith MT, et al. Biomechanical assessment of hip capsular repair and reconstruction procedures using a 6 degrees of freedom robotic system. Am J Sports Med. 2017;45:1745-54.
-
21Wong S, Newhouse A, Chahla J, Nho S. Arthroscopic Treatment of Hip Dislocation After Previous Hip Arthroscopy: Capsular Reconstruction With Labral Augmentation. Arthrosc Tech. 2021 Feb 22;10(3):e867-e872.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- The COVID hangover
- Results of the arthroscopic treatment of acute bony Bankart lesion using the original Porcellini-Sugaya technique and the double-row modified procedure
- Assessment of tibial translation in experimental models of anterior cruciate ligament reconstructions: is dual tibial fixation indicated?
- Learning curve in the arthroscopic Latarjet technique
- Clinical outcomes of the anteromedial technique versus the transtibial technique in reconstruction of the anterior cruciate ligament: a systematic review and meta-analysis of randomized clinical trials
- Basic sciences in reconstruction of the anterior cruciate ligament with the ischiotibial tendons (a narrative review)
- Arthroscopic hip surgery in femoroacetabular impingement
- Circumferential 270º reconstruction of the hip labrum through arthroscopy with knotless tensionable technology Surgical technique
- Arthroscopic capsule reconstruction with dermal mesh plus segmental labral reconstruction with tibialis anterior allograft in recurrent postsurgical hip microinstability
- Synthetic polyethylene mesh augmentation for chronic patellar tendon rupture repair
- The Giant’s Causeway “inside the shoulder”
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.