Update on the diagnosis and treatment of quadriceps muscle injuries
Actualización en el diagnóstico y el tratamiento de las lesiones musculares del cuádriceps
Resumen:
Las lesiones del cuádriceps, tanto las que se producen por mecanismos directos como las que se producen por mecanismos indirectos, son muy frecuentes en la práctica deportiva y tanto su modelo de clasificación como su tratamiento han evolucionado significativamente en los últimos años. Al tratarse de un músculo biarticular, el recto femoral es el componente del cuádriceps que se lesiona con más frecuencia y el que da lugar a mayor variedad de opciones terapéuticas, incluyendo las reparaciones quirúrgicas. Además, el recto femoral está inervado por dos ramas nerviosas motoras separadas que penetran por las zonas proximal y distal del músculo, lo que implicaría una regulación neural diferenciada con papeles funcionales específicos para cada región anatómica sobre la que actúan (cadera o rodilla). Dada su frecuencia y la marcada repercusión funcional que producen, es importante para los traumatólogos conocer las características anatómicas particulares y los modelos de clasificación, diagnóstico y tratamiento actuales de las lesiones del cuádriceps.
Nivel de evidencia: 4 (opiniones de expertos).
Abstract:
Quadriceps injuries secondary to either direct or indirect mechanisms are very common in sports activities, and both their classification and treatment have evolved significantly in recent years. Since it is a biarticular muscle, the rectus femoris is the quadriceps component most often affected by injury and which has a greater variety of treatment options - including surgical repair. In addition, the rectus femoris is innervated by two separate motor branches that penetrate the proximal and distal zones of the muscle - this resulting in differentiated neural regulation with specific functional roles for each anatomical region upon which they act (the hip or knee). Given their frequency and serious functional repercussions, it is important for traumatologists to know the particular anatomical characteristics and current classification, diagnosis and treatment protocols of quadriceps injuries.
Level of evidence: 4 (expert opinions).
Introduction
Quadriceps muscle injuries are a common problem in athletes of all levels. Clear consensus has been established(1) for differentiating between direct and indirect muscle injuries. Because of its structure (with three single-joint muscle bellies and a biarticular muscle belly with a very well defined central tendon or raphe), location and the important demands to which it is subjected in many sports - particularly football - the quadriceps is often affected by both types of injuries, which at present are diagnosed fundamentally on the basis of the ultrasound findings(2). The quadriceps is located on the anterior aspect of the thigh, and its three vastus elements (vastus medialis, vastus lateralis and vastus intermedius) originate on the medial, lateral and anterior surfaces of the femur, respectively. Its biarticular belly, the rectus femoris, originates from three tendons in the proximal anterior region of the coxofemoral joint: the direct tendon, which originates in the anterior inferior iliac spine; the indirect tendon, which originates at the superolateral margin of the acetabulum; and a small reflected portion that inserts in the anterior part of the hip joint. The direct and indirect tendons continue within respective aponeurotic laminas that extend to the lower third of the muscle. The direct tendon continues as the more superficial lamina, while the indirect tendon does so as an intramuscular central lamina(3).
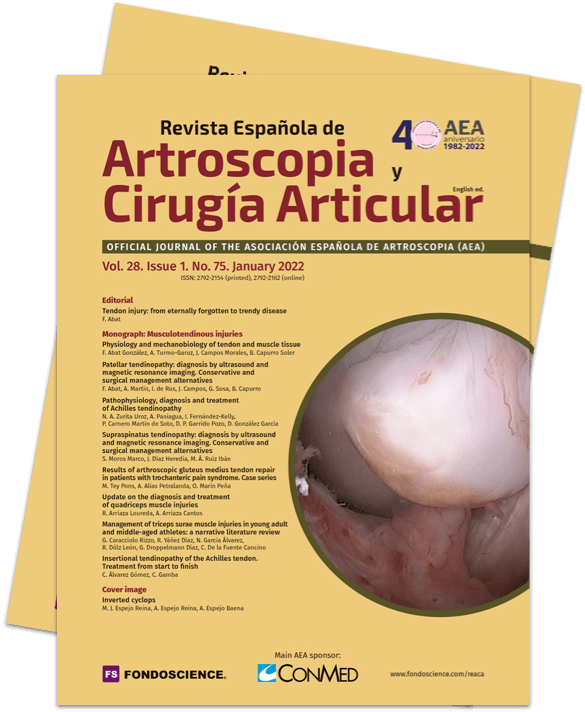
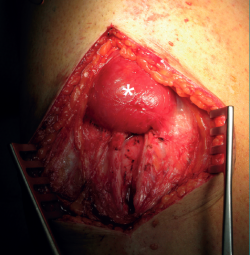
Indirect injuries of the rectus femoris are frequent, in the same way as direct injuries of the vastus medialis and vastus lateralis. Direct injuries are frequent in team sports such as football, rugby or American football, and also in combat sports such as kick-boxing, and usually produce important pain. The ultrasound and magnetic resonance imaging (MRI) studies evidence great destructuring of the muscle tissue, though there is often a surprising dissociation with respect to the clinical manifestations - athletes often being able to continue their sports activities with only minimal limitation despite the lesion(4). Sometimes, and particularly in the occupation setting, we can encounter serious injuries, with muscle sectioning secondary to direct traumatisms, that may require surgical treatment (Figure 1).
reacae.29175.fs1911059en-figure1.png

Figure 1. Right thigh. The head is to the left of the image. Complete sectioning of the vastus medialis, rectus femoris and vastus intermedius caused by the fall of a blunt and very heavy object (the edge of a metal door, from a height), with the knee flexed. Surgical approach for suturing the different muscle bellies.
However, indirect injuries are usually characterized by a long recovery process, and a study carried out among the top teams of the Union of European Football Associations (UEFA) from 2001 to 2013 confirmed that the recovery time is about 20 times longer than in the case of direct injuries(5). We therefore will fundamentally focus on these latter injuries.
On the other hand, in top level football, quadriceps injuries account for 19% of all muscle lesions, and are associated with longer times in returning to sports than injuries of the knee flexor muscles and adductors(6).
The present study offers a descriptive review of quadriceps muscle lesions as an update for traumatologists interested in the field of sports injuries.
Anatomy
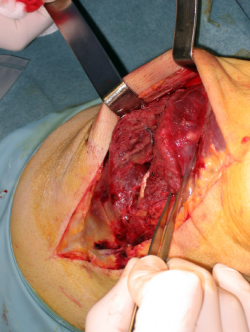
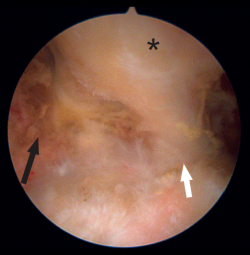
The femoral quadriceps is traditionally considered to be composed of four muscles: the rectus femoris (RF), vastus medialis (VM), vastus lateralis or externus (VE) and the vastus intermedius. However, a number of recent anatomical studies have described different variants of normal, with individuals presenting from 5 to 8 muscle heads(7). Of these, the RF is the only biarticular muscle; thus, in addition to conforming the primary flexor muscle group of the hip, it also extends the knee joint and is exposed to a risk of elevated elongation if movements of both are combined. Due to this characteristic, its length, tendency to perform eccentric-type contractions, and its high percentage of type II fast-twitch fibres, the RF is the quadriceps component most often affected by injuries. Mention also must be made of its complex proximal origin(8), with a direct tendon originating in the anterior inferior iliac spine and a second indirect (or reflected) tendon that originates in the supra-acetabular groove (Figure 2). At approximately 2 cm below their origin, both tendons form a combined tendon structure. The direct portion mainly contributes to the superficial component of the combined tendon and merges with the anterior aponeurosis or fascia of the muscle. In contrast, the indirect portion contributes to the fibres of the deep intramuscular component of the combined tendon and forms a deep musculotendinous junction that extends distally, approximately encompassing the two proximal thirds of the length of the muscle belly of the RF. This deep intramuscular tendon is initially located medially and is "comma" shaped (Figure 3). Distally, the tendon flattens out and becomes linear in shape with a sagittal long axis, and is located more laterally within the muscle(9). This central tendon (also called central aponeurosis or intramuscular septum) in turn gives rise to the muscle fibres that confer the bipennate appearance of this muscle. In turn, the direct tendon gives rise to a superficial expansion that anteriorly covers the proximal part of the muscle, from which muscle fibres also emerge. All the muscle fibres insert in the posterior aponeurotic expansion (posterior fascia) located on the dorsal surface of the muscle, which distally forms the anterior layer of the quadriceps tendon. In this way we have a bipennate structure originating from the central tendon, which differs from another surrounding structure originating from the superficial expansion and which is unipennate. This type of configuration has been referred to as a "muscle within a muscle"(10).
reacae.29175.fs1911059en-figure2.png

Figure 2. Endoscopic view of the tendon of origin of the left rectus femoris. The optics are located anterior to the joint capsule of the hip (which occupies the floor of the image). Note the direct tendon (black arrow) originating in the anterior inferior iliac spine, the reflected tendon (white arrow) originating in the supra-acetabular region, and the combined tendon formed by the joining of the previous tendons (asterisk).
In addition, the RF is innervated by two separate motor branches that penetrate the proximal and distal zones of the muscle - this resulting in differentiated neural regulation with specific functional roles for each anatomical region upon which they act (the hip or knee). In this way the proximal region of the RF exhibits greater amplitude in the surface electromyography (EMG) recordings than the distal and central zones during hip flexion exercises(11), which could possibly explain the tendency towards more frequent injuries in the proximal zone of the RF than in the distal portion.
In this way, muscle injuries may occur in the muscle belly in a myotendinous or myoaponeurotic junction zone. Accordingly, if we accept that the intramuscular tendon acts as a central support for insertion of the muscle fibres, we can understand why muscle damage surrounding it occurs in a "zipper-like" manner and we will see bleeding and edema following the ruptured fibres yielding a characteristic "feather-like" MRI image.
In other cases the lesion may include partial or total rupture of the intramuscular tendon. In such situations it has been seen that the injuries take longer in healing and are moreover more susceptible to relapse(10).
Epidemiology and mechanism of injury
Although injuries of the lower extremity are frequent in different sports, few studies have analysed the frequency and pattern of quadriceps lesions, and most of the available articles are moreover referred to professional football players (6,12). Nevertheless, a recent study has examined their frequency among secondary education athletes and in 25 different sports in the United States (13); the authors concluded that the frequency of quadriceps injuries is approximately one-third that of injuries of the knee flexor muscles, with an incidence (in competition sports of both genders) that is higher in females than in males. Furthermore, the appearance of such injuries is more common in the pre-season period than in the competition season.
In football, the different studies that have analysed the incidence during the season have yielded contradictory results, possibly because of differences in the game surface or in the frequency of matches and training sessions, or in their intensity. In the pre-season of the British Premier League(14) and the Australian Football League(15), RF injuries were more frequent than biceps femoris injuries, while in European football the Ekstrand et al. study recorded no significant differences in frequency during the season(6). As seems logical in view of the functional demands upon the muscle, RF injuries are more common on the dominant side in football players, though no direct correlation has been found with the age of the player - in contrast to injuries in other body locations(15). Curiously, in the same study, Orchard and Seward recorded an inverse relationship between RF injuries and the humidity of the terrain, as well as between the distance/speed of the preparatory run and injuries, more than with the ball striking distance. However, the mentioned study focused on Australian football, which has some characteristics that differ from those of European football. The analysis of the injuries, when affecting the supporting extremity while running, allowed the authors to relate them to deceleration prior to kicking the ball if the stride shortened and the player balanced his trunk backwards, elongating the RF due to its relation to the hip while performing eccentric contraction of the quadriceps in order to slow down. However, experience tells us (Arriaza A., personal communication, June 2019) that RF injuries of the kicking extremity in football players often occur as a result of relatively low-energy actions (e.g., kicking a penalty or in short passing of the ball), in which the player tries to rectify the kick while performing it. We therefore may need to take into account a possible discoordination mechanism that would be favoured by the differential innervation commented above, as a triggering factor - in the same way as may occur in the biceps femoris, where the short portion is innervated from the peroneal nerve and the long portion from the tibial nerve(16).
Due to the mechanism of the injury and its location - exposed to collision with opponents or objects - direct injuries are more frequent in the vastus lateralis and the distal portion of the vastus medialis.
Diagnosis
Ultrasound is an excellent option for studying the muscles that conform the quadriceps and its tendons, provided the operator is sufficiently experienced. Furthermore, ultrasound is the only technique that allows us to evaluate the muscle on a dynamic basis, while MRI provides detailed information on the muscle damage. Despite the advances in imaging diagnosis, it is important to take into account that distinguishing between a direct injury and an indirect injury may prove difficult if based only on the radiological findings. This underscores the usefulness also of the case history in injuries of this kind(17).
Due to the particular characteristics of the quadriceps, with its three single-joint muscle bellies and the biarticular behaviour of the RF - which moreover possesses a central tendon - the traditional muscle injury classifications offer little relevant information for the clinician. The classification of muscle injuries proposed by the Munich consensus(1) does not contemplate the peculiar characteristics of muscles like the RF and the greater tendency towards relapse and longer healing periods and times to return to sports activity in the case of injuries that affect the central tendon.
Other classifications, such as that of the British Athletics Association(18), include consideration of both the anatomical location (myofascial, musculotendinous and intratendinous) and the extent of the lesion in the MRI scan - taking into account not only its longitudinal extent but also its cross-sectional area. However, these classifications do not contemplate either the mechanism producing the injury or whether the injury is of a primary or recurrent nature. Consequently, a new classification has recently been proposed that includes all these parameters and which may be applied to the quadriceps in view of its characteristics, despite the fact that the classification was initially validated for knee flexor muscle injuries(19). This classification (Table 1) includes four main categories that are related to factors that can be of clinical and prognostic importance: the mechanism of the injury (M), the location of the lesion (L), the severity grade (G), and the number of relapses (R). In turn, within category M, we can find direct and indirect injuries and subtypes (S) for lesions caused by stretching and for those produced by speed actions (P). In relation to the location of the injury, three regions are contemplated: proximal, central and distal zone of the muscle belly. In addition, the relation of the injury to the musculotendinous junction zone is taken into account (including the central tendon). Grading of the lesion is based on the MRI images obtained in T2-weighted sequences, where the presence of edema is rated as positive and scored from 1-3 according to its size, while the absence of edema is rated as negative. In addition, if the MRI study evidences an intratendinous lesion, injury affecting the musculotendinous junction, or a lesion showing retraction or loss of tension of the tendon, the classification adds (r) as a superscript. Recurrences (R) correspond to lesions of the same type and which appear in the same location as the initial lesion, during the first two months after returning to competition.
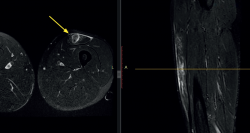
In the case of injuries affecting the intramuscular tendon of the RF, the MRI study often evidences the so-called bull's eye sign, corresponding to an increase in signal intensity around the intramuscular tendon of the RF (Figure 4), that can evolve as the lesion matures from initial edema and bleeding to healing with increased vascularisation around the tendon. A bull's eye sign with atrophy and fat infiltration around the tendon corresponds to an old injury, and we occasionally may observe a pseudocyst due to serohematic fluid accumulation in the rupture zone(20), though this finding is more common in children than in adults.
It is also important to identify another type of injury particular to the RF, namely degloving injury, characterized by an apparent dissociation of the deep component (bipennate) from the surrounding component (unipennate). This dissociation may extend 4-18 cm and occur with or without significant retraction (Figure 5). Since these lesions appear to manifest more often at the periphery of the bipennate internal muscle belly than at the myotendinous junction, they could be defined as injuries of that muscle belly(21).
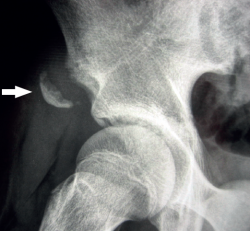
If the pain is located very proximal, it is important to remember that tearing of the tendon may occur at its origin in the anterior inferior iliac spine (AIIS), with or without associated bone avulsion (Figure 6).
Treatment
In general, and as is common in almost all muscle injuries, conservative management is usually prescribed - though there is no specific rehabilitation protocol for RF injuries. It is therefore crucial to take into account the different types of injuries we can find in this muscle in order to adjust the timelines and the functional demands to which it can be exposed, with a view to minimizing the risk of relapse while also avoiding needless delays.
The recovery time until the patient can return to sports activity is shorter in the case of injuries caused by a direct mechanism. In the study of the UEFA(6), indirect lesions required an average of 18.5 ± 19.5 days, while direct injuries allowed the players to return to normal performance after 7.0 ± 9.1 days. However, in some cases, if contusion of the vastus lateralis is very extensive, the recovery period may be very long, particularly because of the difficulty of achieving full flexion of the knee without pain. This has led some authors to recommend immediate initial immobilization with the knee flexed approximately 120º during the first 24 hours after the injury, prescribing crutches for walking without weight bearing until the patient achieves good quadriceps control and can walk without significant pain(22). With this protocol, the authors recorded a mean time to return to sports activity of 6.5 days in the case of mild contusions, 56 days for moderate contusions and 72 days in the case of severe contusions.
It is important to take into account that injuries which affect the central tendon are at a greater risk of relapse and are associated to a longer time to return to sports activity, since repair of the tendon follows a pattern different from that of the muscle lesion. Muscle lesions induce a response on the part of the satellite cells, together with a collagen scaffold on which muscle regeneration takes place, thus allowing faster functional recovery(23). Tendon lesions induce an inflammatory response characterized by the production of extracellular matrix and the appearance of a scar that initially has little resistance to tension and requires the further accumulation of collagen and remodelling - replacing the initial disorganized type III collagen with longitudinally oriented type I collagen - in order to reach a level of resistance sufficient to tolerate activity(24).
Conservative management
Quadriceps injuries secondary to either direct or indirect mechanisms produce bleeding, and a defined hematoma possibly may form among the damaged fibres, followed by an inflammatory reaction. A muscle injury is usually first treated with the protection, rest, ice, compression and elevation (P-RICE) protocol, together with analgesics, and limiting the use of nonsteroidal antiinflammatory drugs (NSAIDs) as far as possible. Evacuation of the hematoma is indicated if it is of significant volume(25). Allowing muscle rest seeks to avoid worsening of the lesion, while the application of ice aims to reduce muscle temperature and lessen blood flow to the injured zone, in order to facilitate faster repair and an earlier return to sports activity - though no supporting evidence is found in the literature(26). In any case, the application of cold has a significant analgesic effect.
Interventional techniques
It should be noted that there are a number of therapeutic procedures, such as the intralesional injection of plasma rich in growth factors or autologous conditioned serum, that could improve or accelerate repair of the RF(27,28), though there is still not enough evidence to recommend their routine use. Nevertheless, the experience gained in many studies centred on the effect of injected plasma rich in growth factors upon the time to return to sports activity in athletes with muscle injuries - including quadriceps lesions - has evidenced time reductions of up to 20% versus control groups(29).
In general, after one week we can start a recovery program consisting of four steps - starting with gentle running and ending with full-power kicking of the ball and running with bursts of acceleration and stopping. The exercises will evolve from very analytical and simple activities to the integration of muscle chains in more complex actions that bring the patient closer to sports performance. In this regard we can adapt the model proposed for injuries of the knee flexor muscles(30). In order to move on to the next level, the athlete must first complete the previous step without discomfort(31). In addition, in our experience and following the methodology also used in biceps femoris lesions, we consider that the subjective feeling of confidence on the part of the athlete is important in deciding to move on to the next level.
The use of MRI for predicting the duration of patient disability is subject to debate. No studies have examined the correlation on a blind basis. As a result, in most cases, visualization of the image of the lesion might have a strong predetermining influence upon the adopted clinical approach and the timelines considered for patient discharge. In fact, the double-blind trial conducted by Moen et al.(32), although focused on hamstring muscle injuries, found that MRI did not contribute additional prognostic information regarding the return to sports activity of the patient. The criteria we use are therefore based on evaluation of the presence or absence of discomfort in response to palpation or isometric contraction of the injured zone; the absence of discomfort on stretching the quadriceps; capacity for speed running, directional changes and - in the case of football players - kicking of the ball; the completion of a progressive sports re-adaptation program including specific actions of the sport at speeds increasingly in line with the real-life demands; and the completion of at least three full trainings with the equipment, in the absence of symptoms.
Surgical treatment
In certain cases, especially those affecting the central tendon of the RF or its tendon of origin, surgical repair of the injury may be needed to resolve the problem. If suturing of the damaged muscle is carried out, subsequent immobilization with the knee extended is important, followed by gradual passive mobilization after three weeks and active mobilization after 6 weeks(33). In the event of tearing of the tendon of origin of the RF, conservative management may be decided, though the time to return to sports activity is long and the relapse rate is in the range of 18%(34). Most authors therefore prefer to reserve conservative management for patients with a low functional demand or non-professional athletes. The series of 10 professional football players operated upon by Vaquerizo et al.(35) comprised 7 acute cases and three patients that underwent surgery between 5-7 months after the initial injury, due to the persistence of symptoms that impeded sports performance at the required level. Surgery was carried out using three different techniques: trans-osseous reinsertion in the acute cases of proximal avulsion; end-to-end suturing in those cases in which rupture occurred at less than 3 cm from the origin; or dissection and mobilization of the distal stump in those cases characterized by great retraction, followed by suturing to the remaining tendon. In addition, repair was supplemented by the application of plasma rich in growth factors. Likewise, Lempainen et al.(36) performed surgical reinsertion through bone anchorings in a series of 19 proximal avulsions of the RF (10 involving both tendons and 9 a single tendon), with good outcomes. The authors therefore recommend this approach in cases of avulsion of both tendons of origin of the RF in patients with high functional demands, or in those subjects in which conservative management has not afforded good results after three months - though they recognize that surgery is technically more simple if performed in the acute phase.
Conclusions
Knowledge of quadriceps muscle injuries has improved in recent years thanks to advances in imaging diagnosis and in our understanding of the anatomy and biomechanical role of the central tendon of the RF. The new classifications of its injuries, while more complex than the classical and simplistic classifications, allow us to advance in the definition of prognostic factors and in the optimization of treatment. The evidence on the role of the new therapies in shortening the healing process and reducing the risk of relapse is still too weak to allow their recommendation on a routine basis, though they have become a common resource in the treatment of athletes - particularly top athletes - where the recovery timelines may be very important.
Figuras
Figure 1. Right thigh. The head is to the left of the image. Complete sectioning of the vastus medialis, rectus femoris and vastus intermedius caused by the fall of a blunt and very heavy object (the edge of a metal door, from a height), with the knee flexed. Surgical approach for suturing the different muscle bellies.
Figure 2. Endoscopic view of the tendon of origin of the left rectus femoris. The optics are located anterior to the joint capsule of the hip (which occupies the floor of the image). Note the direct tendon (black arrow) originating in the anterior inferior iliac spine, the reflected tendon (white arrow) originating in the supra-acetabular region, and the combined tendon formed by the joining of the previous tendons (asterisk).
Figure 3. Axial (T1) view of the thighs, showing the typical "comma" image of the rectus femoris of both quadriceps.
Figure 4. Magnetic resonance imaging scan of the left thigh in axial and sagittal view (T2). Bull's eye sign in a lesion of the left rectus femoris, causing edema around the central tendon and edema of the surrounding muscle tissue (yellow arrow).
Figure 5. Right thigh. The head of the patient lies at the upper part of the image. "Degloving" lesion of the rectus femoris, with characteristic retraction of the proximal stump (asterisk).
Figure 6. Alar radiographic view of the right hip of an adolescent. Apophysiolysis of the anterior inferior iliac spine secondary to traction of the tendon of the rectus femoris of the quadriceps. The arrow indicates the avulsed bone fragment.
Tablas
Información del artículo
Cita bibliográfica
Autores
Rafael Arriaza Loureda
Instituto Médico Arriaza y Asociados. A Coruña
Cátedra HM de Traumatología del Deporte. Universidade da Coruña
Servicio de Cirugía Ortopédica y Traumatología. Hospital Santa Teresa. A Coruña
Instituto Gallego de Cirugía Ortopédica y Traumatología del Deporte. Hospital Santa Teresa. A Coruña
Alvaro Arriaza Cantos
Hospital San Rafael. Madrid
Instituto Médico Arriaza y Asociados
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved studies in humans or in animals.
Data confidentiality. The authors declare that the protocols of their centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Mueller-Wohlfahrt HW, Haensel L, Mithoefer K, et al. Terminology and classification of muscle injuries in sport: the Munich consensus statement. Br J Sports Med. 2013;47:342-50.
-
2Pasta G, Nanni G, Molini L, Bianchi S. Sonography of the quadriceps muscle: examination technique, normal anatomy, and traumatic lesions. J Ultrasound. 2010 Jun;13(2):76-84.
-
3Waligora AC, Johanson NA, Hirsch BE. Clinical Anatomy of the Quadriceps Femoris and Extensor Apparatus of the Knee. Clin Orthop Relat Res. 2009;467:3297-306.
-
4Trojian TH. Muscle contusion (thigh). Clin Sports Med. 2013;32:317-24.
-
5Ueblacker P, Müller-Wohlfahrt HW, Ekstrand J. Epidemiological and clinical outcome comparison of indirect (‘strain’) versus direct (‘contusion’) anterior and posterior thigh muscle injuries in male elite football players: UEFA Elite League study of 2287 thigh injuries (2001–2013). Br J Sports Med. 2015;49:1461-5.
-
6Ekstrand J, Hägglund M, Walden M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39:1226-32.
-
7Olewnik Ł, Tubbs RS, Ruzik K, et al. Quadriceps or multiceps femoris?-Cadaveric study. Clin Anat. 2021 Jan;34(1):71-81.
-
8Soterios G, Zehava Sadka R, Schweitzer M, et al. Normal anatomy and strains of the deep musculotendinous junction of the proximal rectus femoris: MRI features. Am J Roentgenol. 2008;190:W182-6.
-
9Hasselman C, Best T, Hugues C, et al. An explanation for various rectus femoris strain injuries using previously undescribed muscle architecture. Am J Sports Med. 1995;23:493-9.
-
10Balius R, Maestro A, Pedret C, et al. Central aponeurosis tears of the rectus femoris: practical sonographic prognosis. Br J Sports Med. 2009;43:818-4.
-
11Watanabe K, Kouzaki M, Moritani T. Task-dependent spatial distribution of neural activation pattern in human rectus femoris muscle. J Electromyogr Kinesiol. 2012;22:251-8.
-
12Fousekis K, Tsepis E, Poulmedis P, Athanasopoulos S, Vagenas G. Intrinsic risk factors of non-contact quadriceps and hamstring strains in soccer: a prospective study of 100 professional players. Br J Sports Med. 2011;45(9):709-4.
-
13Eckard TG, Kerr TY, Padua TA, et al. Epidemiology of Quadriceps Strains in National Collegiate Athletic Association Athletes, 2009–2010 Through 2014–2015. J Athletic Train. 2017;52(5):474-81.
-
14Woods C, Hawkins RD, Hulse M, et al. The Football Association Medical Research Programme: an audit of injuries in professional football—analysis of preseason injuries. Br J Sports Med. 2002;36:436-41.
-
15Orchard J, Seward H. Epidemiology of injuries in the Australlian Football League seasons 1997–2000. Br J Sports Med. 2002;36:39-44.
-
16Dahmane R, Djordjevic S, Smerdu V. Adaptive potential of human biceps femoris muscle demonstrated by histochemical, immunohistochemical and mechanomyographical methods. Med Biol Eng Comput. 2006;44(11):999-1006.
-
17Kary JM. Diagnosis and management of quadriceps strains and contusions. Curr Rev Musculoskelet Med. 2010;3:26-31.
-
18Pollock N, James SL, Lee JC, et al. British athletics muscle injury classification: a new grading system. Br J Sports Med. 2014;48(18):1347-51.
-
19Valle X, Alentorn-Geli E, Tol JL, et al. Muscle Injuries in Sports: A New Evidence-Informed and Expert Consensus-Based Classification with Clinical Application. Sports Med. 2017;47:1241-53.
-
20Gyftopoulos S, Rosenberg ZS, Schweitzer ME, et al. Normal anatomy and strains of the deep musculotendinous junction of the proximal rectus femoris: MRI features. Am J Roentgenol. 2008;190:W182-6.
-
21Kassarjian A, Rodrigo RM, Santisteban JM. Intramuscular Degloving Injuries to the Rectus Femoris: Findings at MRI. Am J Roentgenol. 2014;202:W475-80.
-
22Aronen JG, Garrick JG, Chronister RD, et al. Quadriceps Contusions: Clinical Results of Immediate Immobilization in 120 Degrees of Knee Flexion. Clin J Sport Med. 2006;16(5):385-7.
-
23Järvinen TA, Järvinen M, Kalimo H. Regeneration of injured skeletal muscle after the injury. Muscles Ligaments Tendons J. 2013;3:337-45.
-
24James R, Kesturu G, Balian G, et al. Tendon: biology, biomechanics, repair, growth factors, and evolving treatment options. J Hand Surg. 2008;33:102-12.
-
25Fernández-Jaén TF, Álvarez Rey G, Ardevol Cuesta J, et al. Spanish Consensus Statement: The Treatment of Muscle Tears in Sport. Orthop J Sports Med. 2015;3(12):2325967115622434.
-
26Bleakley C, McDonough S, MacAuley D. The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sport Med. 2004;32:251-61.
-
27Sheth U, Dwyer T, Smith I, et al. Does Platelet-Rich Plasma Lead to Earlier Return to Sport When Compared With Conservative Treatment in Acute Muscle Injuries? A Systematic Review and Meta-analysis. Arthroscopy. 2018;34(1):281-8.
-
28Wright-Carpenter T, Klein P, Schäferhoff P, et al. Treatment of muscle injuries by local administration of autologous conditioned serum: a pilot study on sportsmen with muscle strains. Int J Sports Med. 2004;25(8):588-93.
-
29Rossi LA, Molina Rómoli AR, Bertona Altieri BA, et al. Does platelet-rich plasma decrease time to return to sports in acute muscle tear? A randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017 Oct;25(10):3319-25.
-
30Valle X, Tol JL, Hamilton B, et al. Hamstring Muscle Injuries, a Rehabilitation Protocol Purpose. Asian J Sports Med. 2015;6(4):e25411.
-
31Cross TM, Gibbs N, Houang M, et al. Acute quadriceps muscle strains: magnetic resonance imaging features and prognosis. Am J Sports Med. 2004;32:710-9.
-
32Moen MH, Reurink G, Weir A, Tol JL, Maas M, Goudswaard GJ. Predicting return to play after hamstring injuries. Br J Sports Med. 2014;48:1358-63.
-
33Shimba LG, Latorre GL, Pochini AC, et al. Surgical treatment of rectus femoris injury in soccer playing athletes: report of two cases. Rev Bras Ortop. 2017;52(6):743-7.
-
34Gamradt SC, Brophy RH. Nonoperative treatment for proximal avulsion of the rectus femoris in professional American football. Am J Sports Med. 2009;37:1370-4.
-
35Vaquerizo García V, Casas Duhrkop D, Seijas R, et al. Surgical treatment of proximal ruptures of the rectus femoris in professional soccer players. Arch Orthop Trauma Surg. 2012;132:329-33.
-
36Lempainen L, Kososla J, Pruna R, et al. Operative Treatment of Proximal Rectus Femoris Injuries in Professional Soccer Players. A Series of 19 Cases. Orthop J Sports Med. 2018;6(10):2325967118798827.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Tendon injury: from eternally forgotten to trendy disease
- Physiology and mechanobiology of tendon and muscle tissue
- Patellar tendinopathy: diagnosis by ultrasound and magnetic resonance imaging. Conservative and surgical management alternatives
- Pathophysiology, diagnosis and treatment of Achilles tendinopathy
- Supraspinatus tendinopathy: diagnosis by ultrasound and magnetic resonance imaging. Conservative and surgical management alternatives
- Results of arthroscopic gluteus medius tendon repair in patients with trochanteric pain syndrome. Case series
- Update on the diagnosis and treatment of quadriceps muscle injuries
- Management of triceps surae muscle injuries in young adult and middle-aged athletes: a narrative literature review
- Insertional tendinopathy of the Achilles tendon. Treatment from start to finish
- Inverted cyclops
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.