Customized 3D printed guides for the repair of rupture of the posterior root of the internal meniscus. Preliminary outcomes
Guías personalizadas impresas en 3D para la reparación de las roturas de la raíz posterior del menisco interno. Resultados preliminares
Resumen:
Objetivo: comparar la funcionalidad de las guías personalizadas impresas en 3D versus las guías estándares comerciales al realizar la reparación de las roturas de la raíz posterior del menisco interno.
Métodos: estudio prospectivo observacional en el que se incluyen 6 pacientes intervenidos artroscópicamente de una reparación de la raíz posterior del menisco interno de la rodilla, divididos en 2 grupos. En uno de ellos se empleó una guía comercial estandarizada y en el otro la guía personalizada impresa en 3D.
Resultados: no hubo diferencias significativas en el tiempo quirúrgico entre ambos grupos (p > 0,05). La media fue de 65 minutos en el grupo estándar (desviación estándar –DE–: 8) y de 63 minutos en el grupo de guías personalizadas (DE: 10). Las guías impresas en 3D se adaptaron en ambos apoyos a la superficie ósea de la tibia y mostraron precisión en la conducción de las agujas guía hacia la posición prevista. No hubo problemas derivados del rozamiento del metal de las agujas con el alma de la guía personalizada y el manejo resultó ergonómicamente satisfactorio para el cirujano.
Conclusiones: de los resultados preliminares obtenidos en este estudio, se puede concluir la viabilidad del diseño y la fabricación de guías personalizadas impresas en 3D para la reparación de las roturas de la raíz posterior del menisco interno, que permitieron realizar los túneles tibiales con precisión. Su empleo no consiguió disminuir el tiempo quirúrgico con respecto a las guías convencionales, aunque permitió una correcta adaptación a la anatomía de los pacientes y una ergonomía satisfactoria para el cirujano.
Nivel de evidencia: nivel 2. Estudio prospectivo de cohortes.
Relevancia clínica: el empleo de guías impresas en 3D permite una cirugía personalizada para la reinserción de la raíz posterior del menisco interno.
Abstract:
Objective: to compare the performance of customized 3D printed guides versus standard commercial guides for the repair of rupture of the posterior root of the internal meniscus.
Methods: a prospective observational study was made of 6 patients subjected to arthroscopic repair of the posterior root of the internal meniscus of the knee. The patients were divided into two groups, with a standard commercial guide being used in one group and the customized 3D printed guide in the other.
Results: there were no significant differences in surgery time between the two groups (p > 0.05). The mean time was 65 minutes in the standard guide group (standard deviation –SD–: 8) versus 63 minutes in the customized guide group (SD: 10). The 3D printed guides adapted on both supports to the bone surface of the tibia and were precise in conducting the guide needles towards the planned position. There were no problems derived from friction between the metal of the needles and the bore of the customized guide, and handling was ergonomically satisfactory for the surgeon.
Conclusions: the preliminary findings of this study warrant the viability of the design and manufacture of customized 3D printed guides for the repair of rupture of the posterior root of the internal meniscus, which allowed precise preparation of the tibial tunnels. Their use did not shorten the surgery time versus the conventional guides, though they allowed correct adaptation to the patient anatomy, and handling was ergonomically satisfactory for the surgeon.
Level of evidence: level 2. Prospective cohort study.
Clinical relevance: The use of 3D printed guides allows customized surgery for reinsertion of the posterior root of the internal meniscus.
Introduction
Rupture of the posterior root of the meniscus is defined as avulsion, with or without a bone fragment, or radial rupture at a location up to 1 cm from its insertion(1). Described in 1991 by Pagnani et al.(2), two presentations have been established based on the underlying etiology: acute traumatic deinsertion affecting the ligament through which the meniscus inserts in the tibia (infrequent and typical of young patients); and degenerative deinsertion (more common) that appears in the context of arthrotic lesions and affects a portion of the meniscus located at a greater distance from the insertion, thereby leaving a posterior stump(3).
Mechanically, these lesions give rise to an alteration similar to total meniscectomy(4), and are also a potential cause of instability of the knee, with rapid progression towards osteoarthrosis of the affected compartment. Their repair restores the load-transmitting function of the meniscus(5,6,7,8,9). Although conservative management and partial meniscectomy have been used with good short-term clinical outcomes(10), repair and reinsertion of the root in its original location is currently the technique of choice.
The method of repair may differ slightly depending on the tear pattern of the root. The surgical reinsertion techniques are divided into two large groups: repair using transosseous sutures and repair using anchorages with suture. The transosseous techniques involve the passing of sutures through the root of the meniscus, recovering them through tunnels drilled in the proximal tibia, followed by knotting them over a post, button or bone bridge on the anterior surface of the tibia(11,12,13,14). Different configurations with different biomechanical properties have been proposed. However, the two simple sutures option has resulted in less displacement of the root and greater rigidity than more complex configurations(15). With regard to the tunnels, single or double tunnel techniques have been described - the latter seeking to better reproduce the anatomical footprint(16).
The transosseous suture techniques require guides for preparing the tibial tunnels through which to reinsert the root. A number of low profile guides are available on the market that are adapted to the laterality of the knee (right or left) and to the meniscus (internal or external). Despite such adaptation, they allow variation of the tunnel angle, but not of the morphology of the intraarticular arm of each of them - a fact that may generate conflicts with the anatomy of certain patients with narrow grooves or prominent spines.
Three-dimensional (3D) printing has been used in knee surgery for the design of customized guides for osteotomy(17) and arthroplasty(18), and even for anatomical positioning of the femoral tunnel in anterior cruciate ligament (ACL) reconstruction surgery(19). However, we have found no mention of application to surgery of the meniscus in the literature.
The present study compares the surgery time, reliability and facility of use of customized 3D printed guides for the repair - using transosseous tunnels - of rupture of the posterior root of the meniscus, adapted to the anatomical characteristics of each patient, versus the standard guides, with the working hypothesis that the former are at least as reliable and ergonomic as the latter, and result in comparatively shorter surgery times.
Material and methods
A prospective observational study was made of 6 patients consecutively operated upon during the year 2020 in our centre to repair the posterior root of the internal meniscus (type 1 and 2 rupture according to the classification of LaPrade)(20), divided into two groups of three patients each. All the patients were operated upon by the same surgeon, and were assigned on an alternating basis to one group or the other. The double tunnel suture guide from Smith & Nephew (Smith & Nephew, Inc., Massachusetts, USA) was used in one group, and the customized 3D printed guide in the other. All patients had been previously diagnosed based on the magnetic resonance imaging (MRI) findings and complied with the indications for transtibial arthroscopic repair (normal axis knee, normal cartilage or with Outerbridge grade I or II lesions and Kellgren-Lawrence grade 0-II lesions). As exclusion criteria, we rejected those patients with associated ligamentous or chondral lesions requiring combined repair procedures.
There were two right knees and one left knee in both groups. In the standard guides group, the mean age was 41 years, with a standard deviation (SD) of three years; all of them were men. In the customized guides group, the mean age was 38 years, with a SD of 5 years; there were two men and one woman. There were no significant differences in age or side of the lesion between the groups.
The study was approved by the Autonomous Clinical Research Ethics Committee, and written informed consent was obtained from all the patients.
Manufacture of the guides was based on virtual reconstruction of the joint using the MITK (Medical Imaging Interaction Toolkit) free access software for the development of medical image processing applications, developed by the Medical and Biological Informatics (MBI) Division of the German Cancer Research Center. As image source, we used the DICOM (Digital Imaging and Communication On Medicine) files corresponding to 1-mm transverse, sagittal and coronal sections of the scan of each patient, obtained with a high-field (1.5 T) Siemens MRI system.
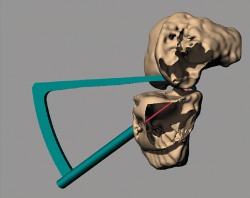
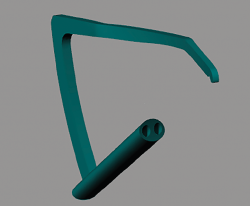
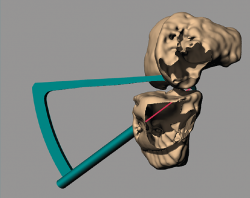
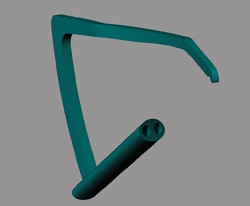
Using Rhinoceros®, Rhino 6 (TLM, Inc.), each guide was designed on a generic basis, followed by adaptation to the virtual reconstruction of the knee of each patient, with an entry point in the anteromedial cortical layer of the tibia located medial to the anterior tibial tuberosity (ATT), adapted to the bone relief, and two exit points in the insertion zone of the posterior horn of the internal meniscus (Figure 1). Each guide housed two 3-mm bores for the creation of two parallel tunnels (Figure 2). The tunnel angle was 60° in all cases, with variation in each case of the morphology of the intraarticular portion of the guide in order to fully adapt it to the anatomy and avoid impacting against the tibial spines or medial femoral condyle.
The virtual image of each knee was printed to create a 3D biological replicate of the joint using a Zortrax® M200 3D printer with high-impact polystyrene (HIPS) as material. Each guide was manufactured using polyamide (a heat-sterilisable material) and an HP® Jet Fusion 4210 printer (Figure 3). The biological replicates allowed virtual surgeries to check the guides for accuracy (Figure 4).
The surgical technique was carried out placing the patient in supine decubitus, following intradural regional anaesthesia, with the knee free on the operating table, a lateral stop and the induction of ischemia using a pneumatic cuff.
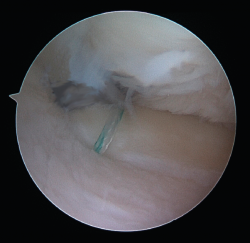
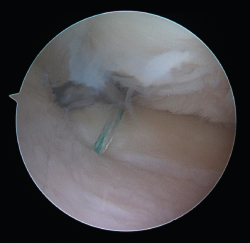
Standard anteromedial and anterolateral portals were used. Once the rupture was identified, the bed of the meniscal root was prepared with an arthroscopic drill, removing the cartilage and leaving a freshened bone base. Using the corresponding guides (Figure 5), two 2.8-mm tunnels were made for passing two number 2 FiberStick® sutures (Arthrex, Inc., Naples, Florida, USA) through one of them. After suturing the meniscus with two simple stitches using a FirstPass® suture passer (Smith & Nephew, Inc., Massachusetts, USA), they were recovered through the other tunnel and knotted onto themselves at the anterior cortical layer of the tibia.
With regard to the statistical analysis, the Student t-test for independent data was used for the comparison of means.
Results
Reinsertion of the meniscal root was achieved in all cases. There were no significant differences in surgery time between the two groups (p > 0.05). The mean surgery time was 65minutes in the standard guide group (SD: 8) versus 63 minutes in the customised guide group (SD: 10).
One of the patients in the standard guide group required modification of the perforation secondary to intraarticular exit of the Kirschner wire in a position different from that planned, due to positioning difficulties caused by the existence of a narrow intercondylar groove and prominent spines. The 3D printed guides adapted on both supports to the bone surface of the tibia and were precise in conducting the guide needles towards the planned position (Figures 6 and 7). There were no problems derived from friction between the metal of the needles and the bore of the customized guide, and handling was ergonomically satisfactory for the surgeon.
Discussion
The present study shows that the use of customized 3D printed guides for the repair of rupture of the posterior root of the internal meniscus did not shorten the surgery time versus the standard commercial guides; our working hypothesis was therefore not confirmed. The customized guides allowed correct adaptation to the anatomy of the patient.
Most commercial manufacturers offer instruments with guides for suturing and preparation of the tibial tunnel or tunnels. Although they facilitate repair and shorten the operating times, meniscal repair guides are not available in all circumstances and are not registered for use in all countries. In addition, they may be expensive, and while modular, their standard design can sometimes cause inconveniences or imprecision in the presence of anatomical variants of the tibia and femur. Low-cost and customized alternatives are therefore required for the treatment of these lesions.
One option for simplifying the process is the design of disposable customized 3D printed guides. The main advantage of 3D printing in medical applications is the capacity to generate customized products(21), templates and accessories tailored to the needs for use in operations, implants, surgical accessories and tools that can be of great value to both patients and surgeons(22).
Additive manufacturing technologies used to be slow and expensive(23). However, proliferation on the market and the progressively lower costs of 3D printers have favoured their accessibility. An important benefit of 3D printing is that it can produce items at a low cost. The traditional manufacturing methods remain less expensive in the context of large scale production, though the cost of 3D printing is increasingly competitive for small productions. Likewise, the speed and software, and the materials used, are continuously being improved upon; as a result, the 3D printing of surgical materials is now a realistic option.
The use of 3D printing to produce single-use instruments offers the possibility of exploring new designs that can change completely from one patient to another, rationalizing the steps in the process.
This approach has been used to manufacture dental, spinal and hip implants(21). In open knee surgery, biological replicates or anatomical models have been manufactured for the treatment of fractures(24), as well as for the production of osteotomy guides(17), arthroplasties(18) and even prosthetic implants(25,26). Surgical guides are the most popular medical application in 3D printing(27). In arthroscopy, this technique has been used to develop guides for anatomical positioning of the femoral tunnel in ACL reconstruction surgery(19). However, we have found no mention of its application to surgery of the meniscus in the literature.
The reported advantages of specific surgical guides for patients include shortened surgery times and greater precision in the operations, thanks to personalisation(28). In the present study, the printed guides were unable to significantly shorten the surgery times, though they were found to be precise tools, and in particular were able to adapt perfectly to the morphology of each of the operated patients. The precision of the guides is an important factor for their generalised adoption in surgery. In a systematic review of the 3D printing techniques in the medical setting, Tack et al.(27) found up to 30% of the models to be associated with average or insufficient precision.
In our study, the opening of the tibial tunnel was seen to be in a favourable position in both groups. However, in one of the cases in which conventional guides were used, a condylar-spinal spatial conflict was observed that resulted in forced positioning of the guide and emergence of the Kirschner wire in a position different from that planned. Repositioning and repeating perforation thus proved necessary.
Customisation of the guide and its adaptation to the anatomy of each individual patient is a clear advantage, particularly in those cases characterized by morphological alterations of the joint. Preoperative planning is facilitated, together with its use in combination with other customized guides in order to avoid the crossing of tunnels in more complex surgeries with associated multiple-ligament damage.
The guides were easy to produce, with a total design and printing time of 24 hours, and a polyamide cost of 8 euros.
The modified MRI protocol with 1-mm sections was necessary to obtain biological replicates guaranteeing the desired precision, and implied another 10 minutes of exploration time. Further studies are needed to determine whether production based on MRI scans of lesser resolution or with a fewer number of imaging acquisitions is feasible.
After sterilisation, these surgical guides can be used intraoperatively in any hospital and may reduce the instruments purchasing costs in those cases where the manufacturers do not supply such instruments along with their implants. On the other hand, these guides not only allow adaptation to the anatomy of the patient but also facilitate ergonomic modifications adaptable to each particular surgeon. Likewise, they weigh less than metal instruments(29).
The limitations of this preliminary study include a small number of patients, which results in low statistical power, and the fact that no evaluation was made of other printers or printable materials capable of improving the accessibility or cost of manufacturing the guides. Lastly, no cost/benefit analysis of the customised guides was made.
Conclusions
This study has demonstrated the viability of the design and manufacture of customized 3D printed guides for the repair of rupture of the posterior root of the internal meniscus, allowing precise preparation of the tibial tunnels.
Their use did not shorten the surgery time versus the conventional guides, though they allowed correct adaptation to the patient anatomy, and handling was ergonomically satisfactory for the surgeon.
Figuras
Figure 4. Printing of the biological replicate allows virtual surgery for assessing the position of the tunnels.
Figure 6. View from the anterolateral portal of the intraarticular positioning of the guide and the intraarticular exit of the tunnels at the footprint of the posterior root of the internal meniscus of a right knee.
Información del artículo
Cita bibliográfica
Autores
Carlos Martín Hernández
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Miguel Servet. Instituto de Investigación Sanitaria (IIS) de Aragón. Zaragoza
Adrián Roche Albero
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Miguel Servet. Instituto de Investigación Sanitaria (IIS) de Aragón. Zaragoza
Miguel Lizcano Palomares
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Miguel Servet. Instituto de Investigación Sanitaria (IIS) de Aragón. Zaragoza
María Durán Serrano
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Miguel Servet. Instituto de Investigación Sanitaria (IIS) de Aragón. Zaragoza
Sara Lairla García
Instituto de Investigación en Ortopedia Avanzada (Younext). Huesca
Antonio Francisco Laclériga Giménez
Departamento de Cirugía Ortopédica y Traumatología. Clínica Universitaria de Navarra. Pamplona
Facultad de Medicina. Universidad de Navarra. Pamplona
Instituto de Ciencias Médicas de Zaragoza (ICM). FREMAP
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Miguel Servet. Instituto de Investigación Sanitaria (IIS) de Aragón. Zaragoza
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has been funded by the aids to research projects of the Fundación Española de Artroscopia in 2019.
Protection of people and animals. The authors declare that this research has not involved studies in humans or in animals.
Data confidentiality. The authors declare that the protocols of their centre referred to the publication of patient information have been followed, and that all the patients included in the study have received sufficient information and have given written informed consent to participation in the study.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Funding and acknowledgements
This study has been funded by the aids to research projects of the Fundación Española de Artroscopia in 2019.
Referencias bibliográficas
-
1Koenig JH, Ranawat AS, Umans HR, Difelice GS. Meniscal root tears: diagnosis and treatment. Arthroscopy. 2009;25(9):1025-32.
-
2Pagnani MJ, Cooper DE, Warren RF. Extrusion of the medial meniscus. Arthroscopy. 1991;7(3):297-300.
-
3Ro KH, Kim JH, Heo JW, Lee DH. Clinical and Radiological Outcomes of Meniscal Repair Versus Partial Meniscectomy for Medial Meniscus Root Tears: A Systematic Review and Meta-analysis. Orthop J Sports Med. 2020;8(11):2325967120962078.
-
4Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922-31.
-
5Choi CJ, Choi YJ, Lee JJ, Choi CH. Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy. 2010;26(12):1602-6.
-
6LaPrade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, LaPrade RF. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96(6):471-9.
-
7Padalecki JR, Jansson KS, Smith SD, et al. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: in situ pull-out repair restores derangement of joint mechanics. Am J Sports Med. 2014;42(3):699-707.
-
8Marzo JM, Gurske-DePerio J. Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am J Sports Med. 2009;37(1):124-9.
-
9Harner CD, Mauro CS, Lesniak BP, Romanowski JR. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Surgical technique. J Bone Joint Surg Am. 2009;91 Suppl 2:257-70.
-
10LaPrade RF, Arendt EA, Getgood A, Faucett SC. The menisci. Berlin, Heidelberg: Springer Berlin Heidelberg; 2017.
-
11Kim YM, Rhee KJ, Lee JK, Hwang DS, Yang JY, Kim SJ. Arthroscopic pullout repair of a complete radial tear of the tibial attachment site of the medial meniscus posterior horn. Arthroscopy. 2006;22(7):795.e1-4.
-
12Raustol OA, Poelstra KA, Chhabra A, Diduch DR. The meniscal ossicle revisited: etiology and an arthroscopic technique for treatment. Arthroscopy. 2006; 22(6):687.e1-3.
-
13Ahn JH, Wang JH, Yoo JC, Noh HK, Park JH. A pull out suture for transection of the posterior horn of the medial meniscus: using a posterior trans-septal portal. Knee Surg Sports Traumatol Arthrosc. 2007;15(12):1510-3.
-
14Nicholas SJ, Golant A, Schachter AK, Lee SJ. A new surgical technique for arthroscopic repair of the meniscus root tear. Knee Surg Sports Traumatol Arthrosc. 2009;17(12):1433-6.
-
15Cerminara AJ, LaPrade CM, Smith SD, Ellman MB, Wijdicks CA, LaPrade RF. Biomechanical evaluation of a transtibial pull-out meniscal root repair: challenging the bungee effect. Am J Sports Med. 2014; 42(12):2988-95.
-
16LaPrade CM, LaPrade MD, Turnbull TL, Wijdicks CA, LaPrade RF. Biomechanical evaluation of the transtibial pull-out technique for posterior medial meniscal root repairs using 1 and 2 transtibial bone tunnels. Am J Sports Med. 2015; 43(4):899-904.
-
17Shen Z, Wang H, Duan Y, Wang J, Wang F. Application of 3D printed osteotomy guide plate-assisted total knee arthroplasty in treatment of valgus knee deformity. J Orthop Surg Res. 2019;14(1):327.
-
18Hooper J, Schwarzkopf R, Fernandez E, et al. Feasibility of single-use 3D-printed instruments for total knee arthroplasty. Bone Joint J. 2019;101-B(7_Supple_C):115-20.
-
19Rankin I, Rehman H, Frame M. 3D-Printed Patient-Specific ACL Femoral Tunnel Guide from MRI. Open Orthop J. 2018;12:59-68.
-
20LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43:363-9.
-
21Mertz L. Dream it, design it, print it in 3-D: what can 3-D printing do for you? IEEE Pulse. 2013;4(6):15-21.
-
22Banks J. Adding value in additive manufacturing: researchers in the United Kingdom and Europe look to 3D printing for customization. IEEE Pulse. 2013;4(6):22-6.
-
23Ventola CL. Medical Applications for 3D Printing: Current and Projected Uses. P T. 2014;39(10):704-11.
-
24Long ZS, Gong FP, Dong XP, Li JT. Clinical application of multiple 3D-printed guide plates for precise reduction and fixation of comminuted patellar fractures. J Int Med Res. 2020;48(11):300060520972088.
-
25Remily EA, Dávila Castrodad IM, Mohamed NS, Wilkie WA, Kelemen MN, Delanois RE. Short-term Outcomes of 3D-Printed Titanium Metaphyseal Cones in Revision Total Knee Arthroplasty. Orthopedics. 2020;7:1-5.
-
26Liu W, Shao Z, Rai S, et al. Three-dimensional-printed intercalary prosthesis for the reconstruction of large bone defect after joint-preserving tumor resection. J Surg Oncol. 2020;121(3):570-7.
-
27Tack P, Victor J, Gemmel P, Annemans L. 3D-printing techniques in a medical setting: a systematic literature review. Biomed Eng Online. 2016 Oct;15(1):115.
-
28Popescu D, Laptoiu D. Rapid prototyping for patient-specific surgical orthopaedics guides: a systematic literature review. Proc Inst Mech Eng H. 2016;230(6):495-515.
-
29Andrés-Cano P, Calvo-Haro JA, Fillat-Gomà F, Andrés-Cano I, Perez-Mañanes R. Role of the orthopaedic surgeon in 3D printing: current applications and legal issues for a personalized medicine. Rev Esp Cir Ortop Traumatol. 2021;65(2):138-51.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Don’t forget to remember
- Anatomical study on subtalar arthrodesis: anterolateral versus posterior portals
- Customized 3D printed guides for the repair of rupture of the posterior root of the internal meniscus. Preliminary outcomes
- Anatomical ligament reconstruction with allograft in chronic acromioclavicular dislocations restores joint stability and function. Short-term outcomes in 14 cases
- Patellar tendinopathy: diagnostic approach and functional assessment scales
- Current management of posterior cruciate ligament rupture. A narrative review
- Management of anterior instability of the shoulder with bone defects
- Open anatomical reconstruction surgical technique with allograft for the treatment of chronic acromioclavicular dislocations
- Simultaneous but different damage to both posterior meniscus roots with multiple ligament injury of the knee following high-energy trauma. Presentation of a case
- Pigmented villonodular synovitis of the ankle
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.