Anatomical study on subtalar arthrodesis: anterolateral versus posterior portals
Estudio anatómico sobre artrodesis subtalar: portales anterolaterales vs. posteriores
Resumen:
Objetivo: analizar el porcentaje de cruentación de la articulación subastragalina (ASA) en muestras cadavéricas con la técnica de artrodesis artroscópica realizada bien por abordajes posteriores o bien por abordajes laterales.
Métodos: estudio descriptivo en el que se realizó una preparación articular artroscópica por portales posteriores en 6 piezas anatómicas de tobillo y en otras 6 más se realizó la técnica por portales laterales. Se consideraron las 3 superficies anatómicas de la articulación subastragalina: posterior (SAP), media (SAM), y anterior (SAA). Se midió y comparó el porcentaje de superficie denudada en las diferentes zonas.
Resultados: los portales artroscópicos posteriores permitieron denudar un 83,6% de la SAP del calcáneo y del 93,7% del SAP del astrágalo. A través de los portales laterales, un 88,8% y un 81,2%, respectivamente, y se pudo denudar un 84,6% de la zona lateral de la SAM del calcáneo y del 83,6% de la homónima del astrágalo. Pero la SAA y las zonas más mediales de la SAM no fueron accesibles desde ninguno de estos portales. El test de Kruskal-Wallis no muestra diferencias significativas en relación con la SAP. La comparación de la SAM cruentada muestra diferencias significativas a favor de los portales laterales (p = 0,02).
Conclusiones: en la muestra estudiada, tanto los portales artroscópicos posteriores como los laterales permitieron un denudado de las superficies articulares posteriores de astrágalo y calcáneo superior al 80%. Los portales artroscópicos laterales permitieron además el acceso y desbridamiento de la SAM con diferencia significativa (p = 0,02). Solamente los abordajes laterales del seno del tarso permitieron poder cruentar también la zona lateral de la SAM. La SAA y la zona medial de la SAM no se pudieron abordar por ninguno de estos portales.
Abstract:
Objective: to analyse the percentage of curettage of the subtalar joint (STJ) in human cadaver samples with the arthroscopic arthrodesis technique adopting either posterior or lateral approaches.
Methods: a descriptive study was made involving arthroscopic joint preparation through posterior portals in 6 anatomical ankle specimens and through lateral portals in another 6 specimens. The three anatomical surfaces of the subtalar joint were considered: posterior (PAS), medial (MAS) and anterior (AAS). Measurement and comparison was made of the percentage of denuded surfaces in the different zones.
Results: the posterior arthroscopic portals allowed denudation of 83.6% of the PAS of the calcaneus and 93.7% of the PAS of the talus. The lateral portals allowed denudation of 88.8% and 81.2%, respectively, together with denudation of 84.6% of the lateral zone of the MAS of the calcaneus and 83.6% of the homonymous surface of the talus. However, the AAS and the more medial zones of the MAS were not accessible from any of these portals. The Kruskal-Wallis test evidenced no significant differences in relation to PAS. Comparison of the MAS following curettage showed significant differences in favour of the lateral portals (p = 0.02).
Conclusions: In the studied sample, both the posterior and the lateral arthroscopic portals allowed over 80% denudation of the posterior joint surfaces of the talus and calcaneus. The lateral arthroscopic portals moreover allowed access and debridement of the MAS, with significant differences (p = 0.02). Only the lateral approaches to the tarsal sinus also allowed curettage of the lateral zone of the MAS. The AAS and the medial zone of the MAS could not be accessed through any of these portals.
Introduction
Tibiotarsal osteoarthrosis is the most frequent presentation of osteoarthrosis within the degenerative disorders of the ankle, and is less often associated to involvement of the subtalar joints. Whether combined or isolated, each of these conditions require specific treatment(1,2). In this respect, subtalar arthrodesis or fixation seeks to achieve solid fusion of the joint in order to eliminate pain and improve function. The most common indication of arthrodesis is painful posttraumatic subtalar osteoarthrosis following fractures of the calcaneus or talus. The indications can be expanded to primary subtalar osteoarthrosis, osteoarthritis following infection, flatfoot osteoarthrosis and other deformities(1,2).
Since the first subtalar arthrodesis procedure in 1912(3), adopting an open lateral and posterior approach, the technique has evolved greatly towards the current arthroscopic fixation techniques(4-22), with Tasto having been the first to describe the arthroscopic procedure(4). The growing interest in arthroscopic techniques is explained by the known benefits they afford in application to other joints: less surgical aggression, improved visualization and access to the structures, and a lesser incidence of complications that allows faster patient recovery. At present, and on the basis of the literature, it seems that most surgeons prefer the arthroscopic technique adopting a posterior approach(7,8,9,10,11).
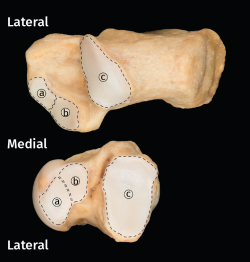
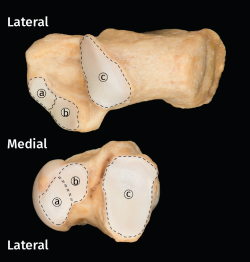
When arthrodesis is performed concomitantly (tibiotalar and subtalar), placing the patient in supine decubitus facilitates the operation. Cleaning and curettage of the subtalar joint (STJ) can be made in this position through two lateral portals in the tarsal sinus. In addition, the use of these lateral portals implies a lesser risk of iatrogenic damage to the surrounding neurovascular structures(23). For improved understanding, it is necessary to clarify that the STJ, comprising the subtalar joint surfaces of the calcaneus and talus, is described as being anatomically composed of three joint surfaces: anterior (AAS), medial (MAS) and posterior (PAS). However, in many cases the cartilage between the anterior and medial surfaces is continuous (Figure 1)(24).
Our working hypothesis is that the denuded surface obtained through curettage of the PAS is the same through both the posterior and the lateral arthroscopic portals. The present study describes the results obtained in relation to percentage denudation of the STJ in human cadaver samples using either the posterior or the lateral arthroscopic portals, in confirmation of the established working hypothesis.
Methods
A descriptive observational study was made involving 12 ankle pieces corresponding to 6 human cadaver specimens, including the complete ankle joint in segments extending from the distal half of the tibia and fibula to the complete foot. It was checked that the specimens had no structural alterations capable of affecting the study. In this regard, one specimen with osteosynthesis material due to fracture had to be replaced. These anatomical pieces were prepared and preserved according to the method of Thiel(25), which allows greater cadaveric joint motion more consistent with that of the original joints. Both genders were equally represented (1:1 proportion), and the mean age was 57 years (range 45-70). Six specimens were assigned to the arthrodesis technique using lateral portals and the other 6 were assigned to the use of posterior portals. The same surgeon, specialized in foot and ankle surgery, performed curettage of the joint surfaces through the usual arthroscopy portals, both lateral and posterior.
Posterior portals technique in prone decubitus
Posterior, posterolateral (PLP) and posteromedial (PMP) portals were prepared following the technique described by van Dijk(22,26). A 5-mm incision was made lateral to the Achilles tendon. The subcutaneous layer was dissected using mosquito forceps, following by placement of the arthroscope with 30° angulation optics in the direction of the subtalar space. The accessory portal was placed medial to the Achilles tendon.
A 30° and 4.0 mm arthroscope (Arthrex, Naples, FL, USA) was used with a hydraulic pressure pump at 40 mm.
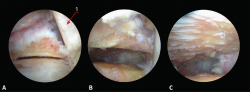
reacae.28373.fs2012052-figure2.png
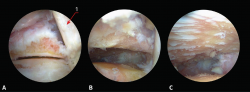
Figure 2. Different steps of the posterior portals arthrodesis technique (left ankle in prone decubitus with viewing through the posterolateral portal). A: visualization of the posterior subtalar joint after synovectomy; B: the same view after debridement of the capsule and fibrous tissue; C: the same view after completing joint cartilage denudation; 1: tendon of the flexor hallucis longus muscle.
Synovectomy was performed using a 4-mm resection synoviotome (Arthrex, Naples, FL, USA). Soft tissue debridement was carried out until the subtalar joint space was located (Figure 2A). The tendon of the flexor hallucis longus muscle served as medial reference.
Following synovectomy and cleaning of the fibrous tissue, the posterior joint surface of the talus and calcaneus was visualized (Figure 2B).
We completed joint debridement and denudation of the cartilage with curettes, scoops and abrasion synoviotomes (Figure 2C), avoiding the creation of large spaces and using the portal exchange manoeuvre.
Lateral portals (tarsal sinus) technique in supine decubitus
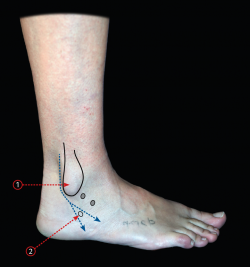
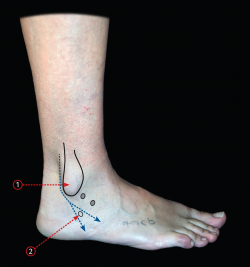
Two lateral portals were prepared, and the technique was performed as described(4). The lateral malleolus and tarsal sinus were used as anatomical references (Figure 3). A 5-mm incision was made 3 mm ahead of the external malleolus and behind the tarsal sinus. The subcutaneous layer was dissected using mosquito forceps, following by placement of the arthroscope with 30° optics obliquely in the direction of the subtalar space. With the arthroscope resting on the bone, the accessory portal was prepared under direct control (Figure 4A).
We used a 30° and 4.0 mm arthroscope with a hydraulic pressure pump at 40 mm.
Synovectomy was performed using a 4-mm resection synoviotome.
Following synovectomy and cleaning of the fibrous tissue, the cervical ligament of the tarsal sinus and the more lateral zone of the MAS corresponding to both the talus and the calcaneus were visualized (Figure 4B). If these ligaments are resected, the more medial zone of the SAM can be seen, though such resection is not indicated in clinical practice.
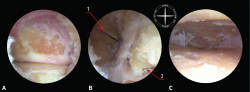
reacae.28373.fs2012052-figure4.png

Figure 4. Different steps of the lateral portals or tarsal sinus arthrodesis technique (left ankle in supine decubitus with viewing through the anterolateral portal). A: visualization of the posterior subtalar joint after synovectomy; B: the same view after debridement of the capsule and fibrous tissue, exposing the cervical ligament of the tarsal sinus; C: the same view after completing joint cartilage denudation. 1: fibular malleolus; 2: fibular trochlea.
Joint cleaning was made with curved curettes and abrasion synoviotomes (Figure 4C), avoiding the creation of large spaces and using the portal exchange manoeuvre.
Quantification of the denuded surface technique
After completing debridement, each specimen was subjected to anatomical disarticulation, exposing the surfaces of the talus and calcaneus. The anatomical areas of the STJ were considered in the exposure (Figure 1)(27): PAS, MAS and AAS, correlating them to the areas that could be accessed with each of the surgical techniques employed. Digital photographs of the surfaces were obtained, and calculation was made of the denuded areas with each of the two techniques, using Image-J image analysing software (Wayne Rasband, National Institutes of Health, Bethesda, MD, USA), in concordance with common practice in studies of this kind(28,29).
Then, measurements were made of the total denuded surface area corresponding to both the talus and the calcaneus; the denuded area working from the PLP and PMP; and the combined area of these two working areas. The same calculations were made in the other 6 specimens in which the lateral portals technique was used. The measurements of the working area were correlated to the total area of the surface of the corresponding joint facet, expressed as a percentage. The Kruskal-Wallis test for the study of variables with a non-normal distribution was used to assess the influence of surface curettage. Statistical significance was considered for p ≤ 0.02.
Results
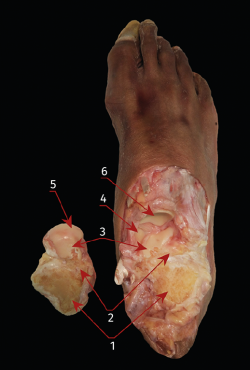
The posterior arthroscopic portals allowed an average surface exposure of 83.6% (range: 73.9-93.5%) of the PAS of the calcaneus and of 93.7% (range: 90.3-95.6%) of the PAS of the talus. However, percentage denudation of the MAS of both the talus and the calcaneus was practically negligible (Figure 5).
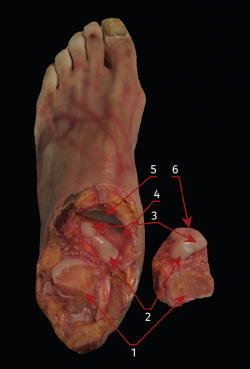
reacae.28373.fs2012052-figure5.png
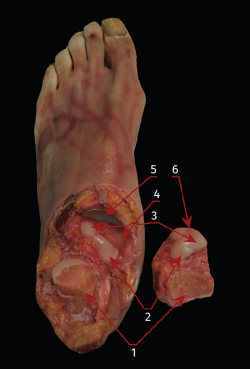
Figure 5. Anatomical dissection showing the joint surfaces of the subtalar joint following arthrodesis through the posterior portals. 1: posterior subtalar joint surface (debrided); 2: medial subtalar joint surface (intact); 3: anterior subtalar joint surface (intact); 4: fibrocartilaginous joint surface of the superomedial calcaneonavicular ligament (part of the spring ligament complex); 5: posterior joint surface of the navicular bone; 6: joint surface of the head of the talus.
The lateral arthroscopic portals in turn allowed an average surface exposure of 88.8% (range: 79.9-91%) of the PAS of the calcaneus and of 81.2% (range: 71.8-92.3%) of the corresponding surface of the talus. Mean percentage denudation of the MAS was 84.6% (range: 74.9-92.8%) of the total joint surface of the calcaneus and of 83.6% (range: 70-92.8%) of the corresponding surface of the talus - though only in the more lateral zones (Figure 6).
reacae.28373.fs2012052-figure6.png
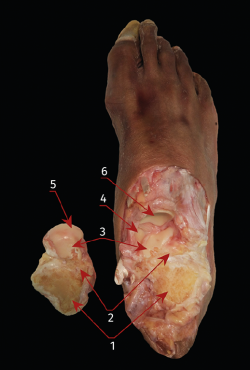
Figure 6. Anatomical dissection showing the joint surfaces of the subtalar joint following arthrodesis through the lateral portals. 1: posterior subtalar joint surface (debrided); 2: medial subtalar joint surface (debrided); 3: anterior subtalar joint surface; 4: fibrocartilaginous joint surface of the superomedial calcaneonavicular ligament (part of the spring ligament complex); 5: joint surface of the head of the talus; 6: posterior joint surface of the navicular bone.
The Kruskal-Wallis test evidenced no significant differences between the two types of approach in relation to the denuded surface. Comparison of the MAS following curettage showed significant differences in favour of the posterior portals (p = 0.02).
Discussion
The results of the present study show that it is possible to denude a similar joint surface of the PAS of both the calcaneus and the talus, using both the posterior and the lateral arthroscopic portals. However, access to the AAS is difficult if not impossible. It also seems difficult to denude the joint areas of the MAS through the posterior portals. In contrast, denudation of over 80% is possible using the lateral technique, but only in the most lateral zone. This could be the explanation for the higher pseudoarthrosis rate described in operated patients when only posterior portals are used, as well as for the longer consolidation time observed with this posterior technique(30,31).
The main contribution of the present study is that it involves a comparative analysis of the two techniques, while other articles are limited to examining one technique or the other(30,31). In their study of 10 specimens using posterior portals, Mouilhade et al.(18) were able to curettage an average of 97.5% of the same posterior joint surfaces, though undoubtedly at the expense of having to perform larger resections; as a result of this, the relief produced by the posteromedial process of the talus impeded adequate coaptation of the prepared surfaces in 8 of the 10 specimens. In our series, we were careful in avoiding such important resections that should not occur in clinical practice, even if the outcome is a lesser percentage of denuded surface. Nevertheless, percentage denudation was always over 60%, which is regarded in the literature as the minimum surface for guaranteeing adequate consolidation(23,32). Similar limitations were found by Lintz et al.(23), who in their case studied 30 cadaver specimens through lateral portals. These authors recorded a percentage preparation of 91.2% in the calcaneus and of 93.9% in the talus, though they likewise described limitations in extrapolating the results to clinical practice, due to the difficulty of finding the limits of debridement of the tarsal sinus and avoiding damage to the peroneal tendons.
The AAS could not be accessed through either of the two techniques. As has been reported, another two accessory portals would be needed for this(31). Access to the medial zones of the MAS also requires the use of accessory medial portals, as commented in the literature(31,). However, this implies a potential increase in the risk of causing neurovascular damage(15,18,28). If it is considered necessary to increase the percentage of denuded surface, we can combine the use of lateral and posterior portals(31), or an accessory portal(8,34).
As limitations of this study, mention should be made of the inherent nature of its design, involving samples from cadavers, and the limited number of specimens involved. Another limitation of studies of this kind is the fact that although the results obtained provide good guidance for surgical practice, no correlation is established, and consequently the data must be supported by the analysis of outcomes in operated patients.
Conclusions
In the studied sample, both the posterior and the lateral arthroscopic portals allowed over 80% denudation of the posterior joint surfaces of the talus and calcaneus. The lateral arthroscopic portals moreover allowed access and debridement of the MAS, with significant differences (p = 0.02). Only the lateral approaches to the tarsal sinus also allowed curettage of the lateral zone of the MAS. The AAS and the medial zone of the MAS could not be accessed through any of these portals.
Figuras
Figure 1. Anatomical view of the subtalar joint surfaces in the calcaneus and talus of a right foot. a: anterior subtalar joint surfaces; b: median subtalar joint surfaces; c: posterior subtalar joint surfaces.
Figure 2. Different steps of the posterior portals arthrodesis technique (left ankle in prone decubitus with viewing through the posterolateral portal). A: visualization of the posterior subtalar joint after synovectomy; B: the same view after debridement of the capsule and fibrous tissue; C: the same view after completing joint cartilage denudation; 1: tendon of the flexor hallucis longus muscle.
Figure 3. Anatomical references for the lateral portals in relation to the lateral malleolus and tarsal sinus; the first 3-mm approach is made immediately behind the tarsal sinus. 1: fibular malleolus; 2: fibular trochlea.
Figure 4. Different steps of the lateral portals or tarsal sinus arthrodesis technique (left ankle in supine decubitus with viewing through the anterolateral portal). A: visualization of the posterior subtalar joint after synovectomy; B: the same view after debridement of the capsule and fibrous tissue, exposing the cervical ligament of the tarsal sinus; C: the same view after completing joint cartilage denudation. 1: fibular malleolus; 2: fibular trochlea.
Figure 5. Anatomical dissection showing the joint surfaces of the subtalar joint following arthrodesis through the posterior portals. 1: posterior subtalar joint surface (debrided); 2: medial subtalar joint surface (intact); 3: anterior subtalar joint surface (intact); 4: fibrocartilaginous joint surface of the superomedial calcaneonavicular ligament (part of the spring ligament complex); 5: posterior joint surface of the navicular bone; 6: joint surface of the head of the talus.
Figure 6. Anatomical dissection showing the joint surfaces of the subtalar joint following arthrodesis through the lateral portals. 1: posterior subtalar joint surface (debrided); 2: medial subtalar joint surface (debrided); 3: anterior subtalar joint surface; 4: fibrocartilaginous joint surface of the superomedial calcaneonavicular ligament (part of the spring ligament complex); 5: joint surface of the head of the talus; 6: posterior joint surface of the navicular bone.
Información del artículo
Cita bibliográfica
Autores
Juan Zaldúa Sáenz de Buruaga
Hospital Universitario de Donostia. San Sebastián
Instituto Vasco de Cirugía Ortopédica-Traumatología (IVCOT). Policlínica Gipuzkoa Quirón-Salud. Donostia-San Sebastián, Gipuzkoa
Servicio de C.O.T. Hospital Donostia. Donostia-San Sebastián. Gipuzkoa
Asier Cuéllar Ayestarán
Instituto Vasco de Cirugía Ortopédica-Traumatología (IVCOT). Policlínica Gipuzkoa Quirón-Salud. Donostia-San Sebastián, Gipuzkoa
Adrián Cuéllar Ayestarán
Instituto Vasco de Cirugía Ortopédica-Traumatología (IVCOT). Policlínica Gipuzkoa Quirón-Salud. Donostia-San Sebastián, Gipuzkoa
Miquel Dalmau Pastor
Unidad de Anatomía Humana. Departamento de Patología y Terapéutica Experimental. Facultad de Medicina. Universidad de Barcelona
GRECMIP-MIFAS (Groupe de Recherche et d’Etude en Chirurgie Mini-Invasive du Pied Minimally Invasive Foot and Ankle Society). Merignac, Francia
Ricardo Cuéllar Gutiérrez
Instituto Vasco de Cirugía Ortopédica-Traumatología (IVCOT). Policlínica Gipuzkoa Quirón-Salud. Donostia-San Sebastián, Gipuzkoa
Ethical responsibilities
Conflicts of interest. The authors declare that they have no conflicts of interest in relation to this article. J.Z. is an occasional remunerated consultant to Arthrex; Ad. C. and R.C. are occasional remunerated consultants to Smith & Nephew.
Financial support. This study was funded in part by a Research Grant from the Fundación Española de Artroscopia in 2016.
Protection of people and animals. The authors declare that the procedures carried out abided with the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentiality. The authors declare that the protocols of their centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Acknowledgements
Thanks are due to the staff of the Department of Surgery, Radiology and Physical Medicine of the Faculty of Medicine and Nursing of the University of the Basque Country (Spain), and particularly to Drs. Ignacio García-Alonso Montoya and Borja Herrero de la Parte, as supervisors of the Experimental Unit and the Surgical Skills Laboratory of the mentioned Department, for their help and collaboration in the present study.
Referencias bibliográficas
-
1Mann RA, Baumgarten M. Subtalar fusion for isolated subtalar disorders. Preliminary report. Clin Orthop Relat Res. 1988;(226):260-5.
-
2Mann RA, Beaman DN, Horton GA. Isolated subtalar arthrodesis. Foot Ankle Int. 1998;19:511-9.
-
3Van Stockum W. Operative behandlung der calcaneus und talusfraktur. Zentralbl Chir. 1912;39:1438-9.
-
4Tasto JP. Arthoscopic subtalar arthrodesis. Tech Foot Ankle Surg. 2003;2:122-8.
-
5Ahn JH, Lee SK, Kim KJ, Kim YI, Choy WS. Subtalar arthroscopic procedures for the treatment of subtalar pathologic conditions: 115 consecutive cases. Orthopedics. 2009;32:891.
-
6Albert A, Deleu PA, Leemrijse T, Maldague P, Devos Bevernage B. Posterior arthroscopic subtalar arthrodesis: ten cases at one-year follow-up. Orthop Traumatol Surg Res. 2011;97:401-5.
-
7Amendola A, Lee KB, Saltzman CL, Suh JS. Technique and early experience with posterior arthroscopic subtalar arthrodesis. Foot Ankle Int. 2007;28:298-302.
-
8Beimers L, de Leeuw PA, van Dijk CN. A 3-portal approach for arthroscopic subtalar arthrodesis. Knee Surg Sports Traumatol Arthrosc. 2009;17:830-4.
-
9Carro LP, Golano P, Vega J. Arthroscopic subtalar arthrodesis: the posterior approach in the prone position. Arthroscopy. 2007;23:445.e1-445.e4.
-
10Glanzmann MC, Sanhueza-Hernández R. Arthroscopic subtalar arthrodesis for symptomatic osteoarthritis of the hindfoot: a prospective study of 41 cases. Foot Ankle Int. 2007;28:2-7.
-
11Lee KB, Park CH, Seon JK, Kim MS. Arthroscopic subtalar arthrodesis using a posterior 2-portal approach in the prone position. Arthroscopy. 2010;26:230-8.
-
12Lee KB, Saltzman CL, Suh JS, Wasserman L, Amendola A. A posterior 3-portal arthroscopic approach for isolated subtalar arthrodesis. Arthroscopy. 2008;24:1306-10.
-
13Lui TH. New technique of arthroscopic triple arthrodesis. Arthroscopy. 2006;22:464.e1-464.e5.
-
14Lui TH. Case report: Correction of neglected club foot deformity by arthroscopic assisted triple arthrodesis. Arch Orthop Trauma Surg. 2010;130:1007-11.
-
15Lui TH, Chan KB, Chan LK. Portal safety and efficacy of anterior subtalar arthroscopy: a cadaveric study. Knee Surg Sports Traumatol Arthrosc. 2010;18:233-7.
-
16Lundeen RO. Arthroscopic fusion of the ankle and subtalar joint. Clin Podiatr Med Surg. 1994;11:395-406.
-
17Mi K, Liu P, Liu W, Feng Z. [Arthroscopical subtalar arthrodesis for malunion of calcaneal fractures]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2010 Jul;24(7):875-7.
-
18Mouilhade F, Oger P, Roussignol X, et al. Risks relating to posterior 2-portal arthroscopic subtalar arthrodesis and articular surfaces abrasion quality achievable with these approaches: a cadaver study. Orthop Traumatol Surg Res. 2011;97:396-400.
-
19Stroud CC. Arthroscopic arthrodesis of the ankle, subtalar, and first metatarsophalangeal joint. Foot Ankle Clin. 2002;7:135-46.
-
20Thaunat M, Bajard X, Boisrenoult P, Beaufils P, Oger P. Computer Tomography assessment of the fusion rate after posterior arthroscopic subtalar arthrodesis. Int Orthop. 2012;36:1005-10.
-
21Tuijthof GJ, Beimers L, Kerkhoffs GM, Dankelman J, Dijk CN. Overview of subtalar arthrodesis techniques: options, pitfalls and solutions. Foot Ankle Surg. 2010;16:107-16.
-
22Van Dijk CN. Hindfoot endoscopy for posterior ankle pain. Instr Course Lect. 2006;55:545-54.
-
23Lintz F, Guillard C, Colin F, Marchand JB, Brilhault J. Safety and efficiency of a 2-portal lateral approach to arthroscopic subtalar arthrodesis: a cadaveric study. Arthroscopy. 2013 Jul;29(7):1217-23.
-
24Badalahu, Qin B, Luo J, Zeng Y, Fu S, Zhang L. Classification of the subtalar articular surface and its matching situation: an anatomical study on Chinese subtalar joint. Surg Radiol Anat. 2020 Oct;42(10):1133-9.
-
25Thiel W. [The preservation of the whole corpse with natural color]. Ann Anat. 1992 Jun;174(3):185-95.
-
26Van Dijk CN, Scholten PE, Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000 Nov;16(8):871-6.
-
27Bartoníček J, Rammelt S, Naňka O. Anatomy of the Subtalar Joint. Foot Ankle Clin. 2018 Sep;23(3):315-40.
-
28Malagelada F, Dalmau-Pastor M, Vega J, Dega R, Clark C. Access to the talar dome surface with different surgical approaches. Foot Ankle Surg. 2019 Oct;25(5):618-22.
-
29Phisitkul P, Tochigi Y, Saltzman CL, Amendola A. Arthroscopic visualization of the posterior subtalar joint in the prone position: a cadaver study. Arthroscopy. 2006 May;22(5):511-5.
-
30Shamrock AG, Amendola A, Glass NA, et al. Do Patient Positioning and Portal Placement for Arthroscopic Subtalar Arthrodesis Matter? Orthop J Sports Med. 2020 Jul 8;8(7):2325967120926451.
-
31Lui TH, Tong SC. Subtalar arthroscopy: When, why and how. World J Orthop. 2015 Jan 18;6(1):56-61.
-
32Ahn JH, Lee SK, Kim KJ, Kim YI, Choy WS. Subtalar arthroscopic procedures for the treatment of subtalar pathologic conditions: 115 consecutive cases. Orthopedics. 2009 Dec;32(12):891.
-
33Lui TH, Chan LK, Chan KB. Medial subtalar arthroscopy: a cadaveric study of the tarsal canal portal. Knee Surg Sports Traumatol Arthrosc. 2013 Jun;21(6):1279-82.
-
34Chinnakkannu K, McKissack H, Alexander B, et al. Subtalar joint preparation using the Two Portal posterior arthroscopic technique versus the sinus tarsi Open approach: A cadaver study. Foot (Edinb). 2021 Mar;46:101690.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Don’t forget to remember
- Anatomical study on subtalar arthrodesis: anterolateral versus posterior portals
- Customized 3D printed guides for the repair of rupture of the posterior root of the internal meniscus. Preliminary outcomes
- Anatomical ligament reconstruction with allograft in chronic acromioclavicular dislocations restores joint stability and function. Short-term outcomes in 14 cases
- Patellar tendinopathy: diagnostic approach and functional assessment scales
- Current management of posterior cruciate ligament rupture. A narrative review
- Management of anterior instability of the shoulder with bone defects
- Open anatomical reconstruction surgical technique with allograft for the treatment of chronic acromioclavicular dislocations
- Simultaneous but different damage to both posterior meniscus roots with multiple ligament injury of the knee following high-energy trauma. Presentation of a case
- Pigmented villonodular synovitis of the ankle
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.