Patellar tendinopathy: diagnostic approach and functional assessment scales
Tendinopatía rotuliana: enfoque diagnóstico y escalas de valoración funcional
Resumen:
Objetivo: realizar una revisión actualizada sobre la tendinopatía rotuliana, centrada en la presentación clínica, el diagnóstico y las escalas de valoración más utilizadas.
Métodos: revisión narrativa de la literatura por parte del Grupo de Estudio de Lesiones Musculares y Tendinosas (GELMUT) de la Asociación Española de Artroscopia (AEA).
Resultados: la tendinopatía rotuliana se manifiesta como un dolor anterior de rótula que evoluciona progresivamente a ser incapacitante. El diagnóstico preciso es vital a la hora de plantear la mejor opción terapéutica y se recomienda realizar confirmación con ecografía; complementariamente, la resonancia magnética ayuda a descartar los diagnósticos diferenciales. El nivel de evidencia de los estudios analizados es de tipo III-IV y permite establecer que para una valoración completa es necesario incluir una escala de valoración global del estado de salud, una de actividad física y 2 específicas de rodilla.
Conclusiones: el diagnóstico se realiza mediante análisis clínico y se confirma mediante ecografía y, en algunos casos, por resonancia magnética. Se recomienda el uso de una escala de valoración global del estado de salud, una de actividad física y 2 específicas de funcionalidad de la rodilla.
Nivel de evidencia: IV (revisión de la literatura de estudios de nivel III-IV).
Abstract:
Objective: providing an updating review on patellar tendinopathy, focusing on the clinical presentation, diagnosis and the most widely used assessment scales.
Methods: a narrative literature review was made by the Muscle and Tendon Injuries Working Group (Grupo de Estudio de Lesiones Musculares y Tendinosas [GELMUT]) of the Spanish Association of Arthroscopy (Asociación Española de Artroscopia [AEA]).
Results: patellar tendinopathy manifests as anterior patellar pain that progresses to the point of becoming disabling. A precise diagnosis is crucial in order to plan the best therapeutic option, and confirmation by ultrasound is advised. On a complementary basis, magnetic resonance imaging helps establish the differential diagnosis with other disorders. The analysed studies presented a level of evidence type III-IV. In order to allow complete evaluation, it is necessary to include a global health assessment scale, a physical activity scale, and two specific knee functional scales.
Conclusions: the diagnosis is established from the clinical analysis and is confirmed by ultrasound and - in some cases - by magnetic resonance imaging. The use of a global health assessment scale, a physical activity scale, and two specific knee functional scales is advised.
Level of evidence: IV (review of the literature corresponding to level III-IV studies).
Introduction
Patellar tendinopathy (also known as jumper's knee) is a disorder of the patellar tendon that includes tendinosis (characterised by a degenerative disease of the tendon as the main underlying causal mechanism) and tendonitis (characterized by inflammation of the tendon) - the latter being regarded as a wrongly used term applied to this disease condition(1). The disorder manifests as well circumscribed pain at the lower pole of the patella and in the anterior zone of the knee(1). The pain is insidious at first and is triggered by physical activity. However, pain gradually becomes more persistent as the frequency and intensity of exercise increase(2).
Patellar tendinopathy accounts for 30-45% of all lesions experienced by jumping athletes(3,4,5,6). The disorder has a strong sports impact, with worrisome data such as those reported by Lian et al.(3), who found that one-third of all athletes requiring treatment because of patellar tendinopathy are unable to return to their sports activity for at least 6 months. It can also affect the occupational activity of non-athletes, with a prevalence of 8-50%, depending on the type of job activity(4). Because of this, it is important to consider that there might be a lack of awareness during diagnostic evaluation, which may prove insufficient and can probably lead to failure of conservative and surgical treatment. In order to define the disorder and describe the most common clinical and therapeutic factors, the European Society of Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA) published a consensus document(5,6) based on the best available clinical evidence, and in the same way as in the present study, the document included articles with a scientific level of evidence III-IV.
The present study comprises a literature review focused on the clinical and imaging diagnosis and the different classifications and functional assessment scales, with a view to presenting the patellar tendinopathy diagnostic evaluation and classification recommendations of the Muscle and Tendon Injuries Working Group (Grupo de Estudio de Lesiones Músculo Tendinosas [GELMUT]) of the Spanish Association of Arthroscopy (Asociación Española de Artroscopia [AEA]).
Medical history and examination
The diagnosis is essentially clinical and is generally based on the medical history and the findings of the physical examination. Correlation between the imaging test data and the clinical evaluation corroborates and guides the diagnosis and the patient recovery process. Patients usually report pain in response to palpation of the deep part of the tendon at the point of its insertion in the lower pole of the patella. The pain is of an insidious nature and generally manifests on starting sports activity. It is important to ask about when the pain starts, since it is a determinant factor in one of the classifications (described further below). Exploration in supine decubitus should be performed with the knee in full extension and the quadriceps femoris muscle relaxed. Positioning the knee in 90º of flexion would increase tension in the tendon, thereby lessening its sensitivity(1). In their systematic review, Morgan et al.(7) underscore that in the physical examination it is important to perform a pain provocation test (single-leg squat test) involving a single-leg squat with the knee in 30° of flexion and the other knee extended (Figure 1), as described by Malliaras et al.(8). This test produces considerable tension in the patellar tendon that in turn causes pain in the presence of tendinopathy. According to Malliaras et al.(8), the load tolerance principle is the most important part of patellar tendinopathy rehabilitation, and is useful for quantifying the results of treatment. Lastly, it is useful to point out that quadriceps atrophy and hypotonia are common findings, and that sudden and rapid contraction of the muscle with the knee in extension can also produce pain due to patellar tendinosis. It must be kept in mind that the patient may present clinical hypersensitivity manifestations even in the absence of any injury identifiable by ultrasound(9).
Diagnostic methods
Ultrasound (US) and magnetic resonance imaging (MRI) are the most common techniques used to visualize the structure of the patellar tendon. Ultrasound presents a sensitivity of 58% and a specificity of 94% in application to patellar tendinopathy, with similar performance in the case of MRI (78% and 86%, respectively)(1,10). However, there is some controversy regarding the use of these imaging tests for the diagnosis of tendon lesions, since it has been seen that the correlation between pain and the structural alterations in tendinopathy is not linear(11). Furthermore, it is not clear whether the structural anomalies seen in the images are predictive of future symptoms or whether they are simply a normal physiological response to specific sports demands that do not indicate an increased risk of future symptoms. In 2016, McAuliffe et al.(12) concluded that structural ultrasound changes are associated to an up to 5-fold increase in the risk of developing tendinopathy, but that other factors are moreover required to trigger the clinical manifestations.
reacae.28373.fs2004023-figure2.png
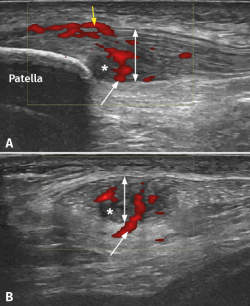
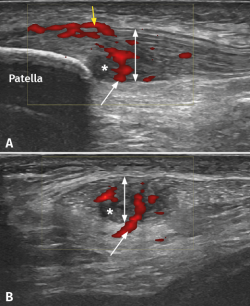
Figure 2. Ultrasound study of proximal patellar tendinopathy. A: longitudinal view of the patellar tendon; B: cross-sectional view of the same tendon. The white arrow shows hypervascularization from Hoffa's fat pad, while the yellow arrow indicates the increase in vascularization at surface (bursa) level. The double white arrow shows the increase in tendon thickness accompanied by hypoechogenic tissue degeneration zones (asterisk).
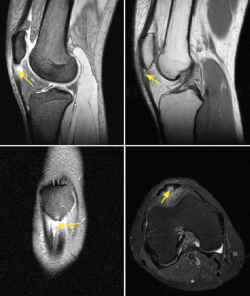
It has been demonstrated that both colour Doppler ultrasound (CD-US) (Figure 2) and MRI (Figure 3) are useful tools for confirming the diagnosis and can orientate treatment(10). Over the last two decades, ultrasound tissue characterization (UTC) has been developed with the purpose of obtaining even more information than conventional ultrasound. Indeed, the technique has become so important that some authors consider that UTC could be the most important development in medical US imaging since the introduction of Doppler ultrasound(13). Ultrasound tissue characterization is an imaging technique specifically designed for application to tendons. It is based on a colour scale that allows us to determine the degree of elasticity of the tendon tissue, and is able to measure small changes in tendon structure (e.g., as in evaluating the presence of tissue degeneration or fibrosis) - allowing us to establish an early diagnosis that can limit chronification of the process. The technique also has therapeutic applications as a tool for monitoring and guiding ongoing treatments, even after surgical repair, or for measuring the time for returning to physical activity (particularly in top athletes)(14,15).
Classification
A number of classifications can be found in the current literature. As a simplification, and to facilitate understanding, the existing tools can be divided into clinical- and imaging-based (using US and MRI) classifications. Some authors advocate classifying patellar tendinosis according to the Victorian Institute of Sport Assessment – Patella (VISA-P) score(16). This functional evaluation and monitoring scale will be explained in the section corresponding to functional assessment scales.
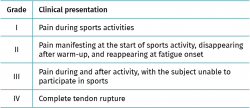
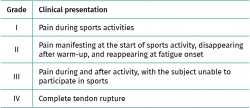
Classification of Blazina
Introduced by Blazina et al.(17) in 1973, this classification provides a qualitative description of the clinical progression of a patellar tendon injury. The different phases are described in Table 1. Roels et al.(18) subsequently modified phase 4, which represents complete tendon rupture.
Classification according to the duration of symptoms
Other authors such as Kaux et al.(19) recommend the classification of patellar tendinopathy as follows:
- Acute: symptoms duration between 0-6 weeks of evolution.
- Subacute: symptoms duration between 6-12 weeks.
- Chronic: symptoms duration > 3 months of evolution.
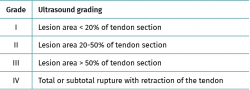
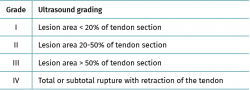
Classification according to lesion area
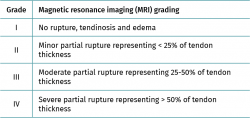
Gemignani et al.(20) classified patellar tendon lesions according to the percentage of damaged area. This is an ultrasound-based classification comprising four grades (Table 2).
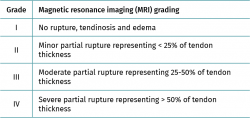
Classification according to the magnitude of tendon rupture
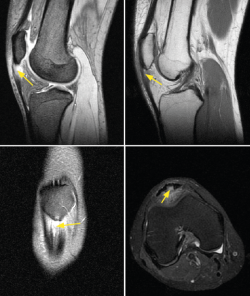
A recent study by Golman et al.(21) has classified patellar intratendinous lesions as corresponding to either partial or total rupture (Table 3). This classification is based on the MRI findings.
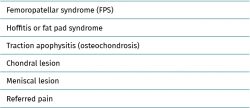
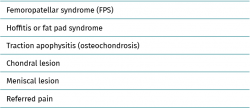
Differential diagnosis
Since the patellar tendon is an anatomical structure intimately related to the biomechanics of the knee, an analysis and study of the rest of the joint structures will be needed in order to establish a correct and detailed differential diagnosis (Table 4). In this regard, patellar tendinosis must be differentiated from:
Femoropatellar syndrome (FPS)
This syndrome is the most common cause of anterior knee pain(1). The condition is triggered by an alteration of patellar tracking within the trochlear sulcus, that can be influenced by a number of factors. The anatomical factors include trochlear width, inclination or patellar tilt. Biomechanical factors of the lower extremities also exert an influence, such as the femoral anteversion angle, measurement of the Q angle, genu valgus, recurvatum, tibia vara or foot pronation, among others. Mention also must be made of the muscular factors, such as weakness of the abductor and external rotator muscles of the hip, as well as of the knee extensor muscles. Lastly, a lack of elasticity of the flexor muscles of the hip and flexion-extension muscles of the knee also exert an influence (22). Seventy percent of all patients over 40 years of age with femoropatellar pain present a variable degree of osteoarthrosis of the joint(23), and this also may be concomitant to patellar tendinopathy. Clinically, the patient suffers mechanical pain associated to crepitation and variable limitation of daily living and sports activities. The diagnosis is established from the physical examination, and complementary confirmation tests are usually not necessary(24).
Fat pad syndrome
Fat pad syndrome is caused by impingement of the infrapatellar adipose tissue or Hoffa's fat pad on the anterior surface of the femur or tibia. The clinical manifestations are similar to those of FPS, and the disorder is more frequent in women between 30-40 years of age that perform repeated jumping exercises. The syndrome manifests as anterior knee pain that increases especially on walking up and down stairs, and may be associated to risk factors for this disorder (femoropatellar dysplasia, knee laxity and/or genu recurvatum(25). The diagnosis is based on the clinical and MRI findings(26). In the early 20th century, the orthopedic surgeon Albert Hoffa(27) described a diagnostic test that may be of interest: with the patient in supine decubitus and from a position of 90° flexion of the knee, we palpate the anterolateral part of the knee and, if pain manifests in the last 10° of extension, the sign is considered to indicate disease suggestive of inflammation of the infrapatellar fat pad.
Traction apophysitis
This disorder is generally found in pediatric patients. In relation to the insertions of the patellar tendon, we can find the following conditions: Osgood-Schlatter disease (in which the anterior tibial tuberosity [ATT] is affected) and Sinding-Larsen-Johansson syndrome (in which the lower pole of the patella is affected)(28). Osgood-Schlatter disease occurs as a result of repeated traction of the patellar tendon upon the ATT. It typically manifests during the peak growth period between approximately 8-13 years of age in girls and 10-15 years of age in boys, especially if the patient participates in sports that involve repeated jumping or continuous running(29). The diagnosis is established from the case history and physical examination. No complementary imaging tests are generally needed, though the presence of alarm symptoms such as nocturnal pain or a history of trauma would justify their use, and in this regard ultrasound affords very valuable information and is moreover noninvasive(30). On the other hand, the appearance of this disease condition in adults is related to direct trauma to the ATT(30).
Sinding-Larsen-Johansson syndrome shares clinical, diagnostic and therapeutic characteristics with Osgood-Schlatter disease, though in the former case the affected zone is the lower pole of the patella(31).
Chondral and/or meniscal lesions
Certain intraarticular injuries can cause pain similar to that of patellar tendinopathy, such as femoropatellar chondral lesions or anterior horn meniscal rupture. Radiographic joint cartilage modifications have been found in 4-10% of all patients between 15-24 years of age - a figure that reaches 80% in individuals over 55 years of age. Likewise, two out of every three knee arthroscopies evidence pathological chondral changes(28,32). Chondral lesions are clinically characterized by pain, effusion and mechanical symptoms. The pain behaves differently depending on the location of the lesion, and is more common when kneeling down, in maximum knee flexion positions, or on walking up stairs in patellar involvement, while in the case of femoral lesions the pain worsens with impact-generating activities. The diagnosis requires a full radiographic study, including axial views of the patella, and an MRI scan. A case series(33) study has described the appearance of lateral meniscus lesions and femoropatellar joint chondropathy, as well as Hoffa's fat pad disorders and synovial hypertrophy, in patients with chronic patellar tendinopathy.
Referred pain
A number of disorders can produce referred anterior knee pain without actual knee disease. For this reason, the physical examination of patellar tendinopathy must include a physical examination of the hip, since disorders such as adult coxarthrosis(34), Cam morphology femoroacetabular impingement, Perthes disease or proximal femoral epiphysiolysis in pediatric patients(35) can manifest as knee pain.
Functional assessment scales
Functional assessment scales are essential for ensuring a complete first diagnostic appraisal, since they include objective and subjective measurements that allow us to assess the patient course over time following therapeutic intervention.
Such scales examine objective parameters such as general health, pain and range of joint motion, among others, and also contribute subjective information such as patient satisfaction and expectations before and after treatment.
In order to perform a correct evaluation based on validated questionnaires, it is advisable to use at least one global health assessment scale, a pre-/post-injury physical activity score, and two scales specific of the disease condition requiring treatment(36).
Generic questionnaires for assessing health condition
The Short Form-36 (SF-36) offers a general perspective of the patient health condition and allows us to calculate the health-related quality of life profile. This tool consists of 36 multiple response questions that explore 8 different health dimensions (physical function, limitation due to physical problems, bodily pain, social function or role, mental health, limitation due to emotional problems, vitality, energy or fatigue, and general health perception), allowing joint assessment or the assessment of each concrete domain independently. The scores of each of the 8 dimensions of the SF-36 range between 0-100, where 100 indicates optimum health and 0 indicates very poor health. The responses assess the patient health condition of the previous month, and a second version has been developed that assesses the previous week. One of the inconveniences of this instrument is complexity in calculating the statistical result(37), though the questionnaire allows us to detect variations in health condition in multiple clinical disorders, and is the most widely used global health measure in orthopedic surgery and traumatology research(38). The SF-36 has a validated version translated into Spanish, which further facilitates its administration in our setting(39,40).
The Short Form-12 (SF-12) is the short (12 questions) version of the SF-36. It also allows calculation of the global health condition of the patient, and its main advantage is that it takes less time for the patient to complete - thereby facilitating its application. However, it is less potent than the original extended version, and does not allow us to obtain measures of the different health dimensions independently(36,40).
The Nottingham Health Profile is a questionnaire consisting of 38 yes/no questions. It is therefore easy for the patient to complete and is easy to analyse, since the result is a single overall score, which facilitates statistical use. The tool moreover has a second part comprising 7 questions referred to patient daily life(41). Its disadvantage in relation to the SF-36 is that it only assesses health/disease and does not allow us to study each domain independently. It has been used particularly in patients with osteoarthrosis of the lower extremities(36).
The EuroQoL was designed to complement other forms of measuring quality of life, and was specifically developed to generate a cardinal health index, which affords considerable potential for use in patient evaluation(42). The first part of the EuroQoL consists of 15 questions with three possible answers that explore mobility, personal care, daily activities, pain and depression, while the second part consists of a visual analogue scale for the assessment of patient global health perception(38). There is a validated version translated into Spanish, which facilitates its use in our setting(43).
Specific questionnaires for assessing knee disease and patellar tendinopathy
A range of functional assessment scales are available, specifically designed for application to knee function and pain. Considering that the symptoms of patellar tendinopathy are difficult to quantify, the current recommendation is to use two different subjective scales together with an objective assessment in the physical examination based on the pain provocation test(7).
The Victorian Institute of Sports Assessment for Patellar Tendinopathy (VISA-P) is the most widely used subjective scale for assessing patellar tendinopathy(16). This disease-specific clinical scale has been validated for patellar tendinopathy and contributes to its functional assessment(44). The VISA-P allows clinical classification based on the severity of symptoms, functional capacity and sports capacity, and helps both the healthcare team and the patient to quantify progress. In addition, it allows the early detection of any worsening of the symptoms. This tool consists of 8 items with a score ranging from 0-100 points. Optimum condition is represented by a score of 100. The validated version in Spanish of the VISA-P can be consulted at: https://www.jospt.org/doi/pdf/10.2519/jospt.2011.3613(45,46).
The visual analogue scale (VAS) is used to measure pain sensation as reported by the patient. This is a subjective, unidimensional and sensitive instrument that estimates pain intensity in disease conditions(44,47). Considered independently, these measurements are valid and reliable in application to many clinical settings - including the rehabilitation of patients with patellar tendinopathy(46,48). The VAS measures patient pain at the start and during rehabilitation, and offers precise evaluations of the intensity of pain and of variations in pain(44).
The combined administration of the VAS and of VISA-P is recommended, since both instruments are widely used in the rehabilitation of patients with patellar tendinopathy.
The other scales that have been proposed in the literature to complement the assessment of patellar tendinopathy are the Tegner activity scale, the International Knee Documentation Committee Knee Form (IKDC), the Kujala scale and the Knee Society Score (KSS).
The Tegner activity scale(49) is a subjective satisfaction score in which the patient rates his or her personal perception of general function of the operated knee. The activity level is scored from 0-10, where 10 is perfect (0 = disability; 1-4 = no physical activity, but able to work; 5-7 = leisure physical activity; 7-10 = competition physical activity). The scale arbitrarily groups sports activities into different levels without considering the frequency of such activities. Although the Tegner scale has not been statistically validated for use in Spanish and for reliability, it remains widely employed as a complementary assessment test(50).
The International Knee Documentation Committee Knee Form (IKDC) was developed in 1987, and one of its main objectives was the administration of a simple questionnaire that is easy to use and which can be employed to evaluate different disorders of the knee, including ligamentous, meniscal, patellofemoral and osteoarthrosis lesions. In addition, it allows the comparison of different groups with different diagnoses(51,52). The IKDC combines symptoms and signs. Each category is globally classified as A (normal), B (near normal), C (abnormal) or D (severely abnormal). The final evaluation of A, B, C or D is determined by the poorest score. This method comprises a subjective part of 18 questions that take into account the symptoms, sports activities and function. The scores are added and transformed into a scale from 0-100. The clinical evaluation part of the IKDC is divided into two sections: the first documents range of motion, the position of the patella, alignment of the knee and joint laxity. The second section in turn is divided into 7 groups (inflammation, limitation of passive motion, ligament assessment, compartmental findings, morbidity of the graft donor site, radiographic findings and functional test). The final result is determined by the lowest result of the group, in theory because the knee must be normal in order to achieve a perfect score. The IKDC has been validated for a range of conditions of the knee, including ligament, meniscal and joint cartilage injuries(53,54,55). It has also been standardized for different ages and genders(56).
The Kujala scale assesses pain and function in patients with patellofemoral joint disorders(57). It consists of 13 questions, each with 3 to 5 possible answers, scored from 0-5 or from 0-10, depending on the question. The lowest possible total score is 0 and corresponds to patients in poorer health functional condition. The highest possible total score is 100 and corresponds to patients with no alterations and who are in optimum conditions. This instrument has been validated in its Spanish version(58) and can be consulted at: http://www.scielo.org.co/pdf/cesm/v31n1/0120-8705-cesm-31-01-00047.pdf.
The Knee Society Score (KSS) has been developed by the American Knee Society. The Knee Society Clinical Rating System has evolved over time: the original version was modified by Insall(59), and this was followed by further changes to add new aspects and to simplify the tool, though preserving its integrity over time(60). At present, this is a scale where both the patient and the surgeon participate in the evaluation. It consists of a first knee score from 0-100 that evaluates pain, stability and range of motion (where 0 is the poorest score and 100 the best score), and a second score corresponding to knee function, with the same 0-100 scoring system. The surgeon completes the objective knee score, which includes a VAS score of pain on walking over a levelled surface, slopes or stairs, and also an evaluation of alignment, stability of the ligaments and the range of motion of the joint. Posteriorly, the patients record their degree of satisfaction, functional activities and expectations. This tool may present some interobserver variation. At present, it is the internationally most widely used assessment scale in knee replacement surgery(36), and has been validated in its Spanish version(61); it can be consulted at: https://link.springer.com/article/10.1007/s00167-013-2412-4.
Conclusions
Diagnostic approach
In patients with anterior knee pain, the medical history and physical examination suffice to establish the diagnosis. It is advisable to include a pain provocation test in the physical examination(8), consider differential diagnoses, and complement the study with diagnostic tests such as ultrasound, which allows us to confirm the diagnosis and classify the tendinopathy. Magnetic resonance imaging is indicated if the patient symptoms persist and ultrasound is unable to identify relevant findings.
Classification
Of the different proposed classifications, the clinical classification of Blazina is recommended, complemented by ultrasound-based classifications in view of their similar performance and lesser cost, and secondarily with MRI-based instruments. Both offer detailed information about the condition of the injury and its clinical course.
Assessment scales
The use of a global health assessment scale (SF-36), a pre-/post-lesion physical activity scale, and two specific knee functional scales (VISA-P and KSS) is advised.
Figuras
Figure 1. Single-leg squat test. A squat is performed with the patient knee in 30° flexion and the other knee extended. This test produces considerable tension in the patellar tendon that causes pain in the presence of tendinopathy(8).
Figure 2. Ultrasound study of proximal patellar tendinopathy. A: longitudinal view of the patellar tendon; B: cross-sectional view of the same tendon. The white arrow shows hypervascularization from Hoffa's fat pad, while the yellow arrow indicates the increase in vascularization at surface (bursa) level. The double white arrow shows the increase in tendon thickness accompanied by hypoechogenic tissue degeneration zones (asterisk).
Figure 3. Magnetic resonance imaging (MRI) view of a patient with long-evolving patellar tendinopathy. Note thickening of the tendon in the sagittal and coronal views, as well as internal destructuring of the collagen fibers (marked by arrows).
Tablas
Información del artículo
Cita bibliográfica
Autores
Ferrán Abat González
Traumatólogo deportivo, ReSport Clinic Barcelona.
Universidad Blanquerna, Ramon Llull. Barcelona
Servicio de Cirugía Ortopédica y Traumatología. Hospital de la Santa Creu i Sant Pau. Universitat Autònoma de Barcelona
Bruno Capurro
ReSport Clinic Barcelona. Universidad Blanquerna, Ramon Llull. Barcelona
Ignacio de Rus Aznar
Servicio de Cirugía Ortopédica y Traumatología. Clinica CEMTRO. Madrid
Unidad de Hombro y Codo. Hospital Universitario Ramón y Cajal. Madrid
Servicio de Cirugía Ortopédica y Traumatología. Hospital Monográfico Asepeyo Coslada. Madrid
Hospital Universitario de Torrejón. Madrid
Adrián Martín Martínez
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Miguel Servet. Zaragoza
Jocelio Campos Moraes
ReSport Clinic Barcelona. Universidad Blanquerna, Ramon Llull. Barcelona
Gustabo Sosa
ReSport Clinic Barcelona. Universidad Blanquerna, Ramon Llull. Barcelona
Unidad de Medicina Deportiva. Hospital Universitario Quirón Dexeus. Barcelona
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved experiments in humans or in animals.
Data confidentiality. The authors declare that the protocols of their centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Figueroa D, Figueroa F, Calvo R. Patellar Tendinopathy: Diagnosis and Treatment. J Am Acad Orthop Surg. 2016;24(12):e184-92.
-
2Cook JL, Khan KM, Kiss ZS, Griffiths L. Patellar tendinopathy in junior basketball players: a controlled clinical and ultrasonographic study of 268 patellar tendons in players aged 14-18 years. Scand J Med Sci Sports. 2000;10(4):216-20.
-
3Lian OB, Engebretsen L, Bahr R. Prevalence of jumper’s knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med. 2005;33(4):561-7.
-
4Van der Worp H, Zwerver J, Kuijer PPFM, Frings-Dresen MHW, van den Akker-Scheek I. The impact of physically demanding work of basketball and volleyball players on the risk for patellar tendinopathy and on work limitations. J Back Musculoskelet Rehabil. 2011;24(1):49-55.
-
5Abat F, Alfredson H, Cucchiarini M, et al. Current trends in tendinopathy: consensus of the ESSKA basic science committee. Part I: biology, biomechanics, anatomy and an exercise-based approach. J Exp Orthop. 2017;4(1):18.
-
6Abat F, Alfredson H, Cucchiarini M, et al. Current trends in tendinopathy: consensus of the ESSKA basic science committee. Part II: treatment options. J Exp Orthop. 2018;5(1):38.
-
7Morgan S, Coetzee FF. Proposing a patellar tendinopathy screening tool following a systematic review. South Afr J Physiother. 2018;74(1):454.
-
8Malliaras P, Cook J, Purdam C, Rio E. Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. J Orthop Sports Phys Ther. 2015;45(11):887-98.
-
9Cook JL, Khan KM, Kiss ZS, Coleman BD, Griffiths L. Asymptomatic hypoechoic regions on patellar tendon ultrasound: A 4-year clinical and ultrasound followup of 46 tendons. Scand J Med Sci Sports. 2001;11(6):321-7.
-
10Warden SJ, Kiss ZS, Malara FA, Ooi ABT, Cook JL, Crossley KM. Comparative accuracy of magnetic resonance imaging and ultrasonography in confirming clinically diagnosed patellar tendinopathy. Am J Sports Med. 2007;35(3):427-36.
-
11Malliaras P, Cook J, Ptasznik R, Thomas S. Prospective study of change in patellar tendon abnormality on imaging and pain over a volleyball season. Br J Sports Med. 2006;40(3):272-4.
-
12McAuliffe S, McCreesh K, Culloty F, Purtill H, O’Sullivan K. Can ultrasound imaging predict the development of Achilles and patellar tendinopathy? A systematic review and meta-analysis. Br J Sports Med. 2016;50(24):1516-23.
-
13Winn N, Lalam R, Cassar-Pullicino V. Sonoelastography in the musculoskeletal system: current role and future directions. World J Radiol. 2016;8(11):868-79.
-
14Van Schie HTM, de Vos RJ, de Jonge S, et al. Ultrasonographic tissue characterisation of human Achilles tendons: quantification of tendon structure through a novel non-invasive approach. Br J Sports Med. 2010;44(16):1153-9.
-
15Van Ark M, Rabello LM, Hoevenaars D, et al. Inter- and intra-rater reliability of ultrasound tissue characterization (UTC) in patellar tendons. Scand J Med Sci Sports. 2019;29(8):1205-11.
-
16Visentini PJ, Khan KM, Cook JL, Kiss ZS, Harcourt PR, Wark JD. The VISA score: an index of severity of symptoms in patients with jumper’s knee (patellar tendinosis). Victorian Institute of Sport Tendon Study Group. J Sci Med Sport. 1998;1(1):22-8.
-
17Blazina ME, Kerlan RK, Jobe FW, Carter VS, Carlson GJ. Jumper’s knee. Orthop Clin North Am. 1973;4(3):665-78.
-
18Roels J, Martens M, Mulier JC, Burssens A. Patellar tendinitis (jumper’s knee). Am J Sports Med. 1978;6(6):362-8.
-
19Kaux JF, Forthomme B, Goff CL, Crielaard JM, Croisier JL. Current opinions on tendinopathy. J Sports Sci Med. 2011;10(2):238-53.
-
20Gemignani M, Busoni F, Tonerini M, Scaglione M. The patellar tendinopathy in athletes: a sonographic grading correlated to prognosis and therapy. Emerg Radiol. 2008;15(6):399-404.
-
21Golman M, Wright ML, Wong TT, et al. Rethinking Patellar Tendinopathy and Partial Patellar Tendon Tears: A Novel Classification System. Am J Sports Med. 2020;48(2):359-69.
-
22Mellinger S, Neurohr GA. Evidence based treatment options for common knee injuries in runners. Ann Transl Med. 2019;7(Suppl 7):S249.
-
23Crossley KM, Callaghan MJ, van Linschoten R. Patellofemoral pain. Br J Sports Med. 2016;50(4):247-50.
-
24Van Linschoten R, van Middelkoop M, Berger MY, et al. Supervised exercise therapy versus usual care for patellofemoral pain syndrome: an open label randomised controlled trial. BMJ. 2009;339:b4074.
-
25Eymard F, Chevalier X. Inflammation of the infrapatellar fat pad. Joint Bone Spine. 2016;83(4):389-93.
-
26Maurel B, Le Corroller T, Cohen M, et al. [Infrapatellar fat pad: anterior crossroads of the knee]. J Radiol. 2010;91(9 Pt 1):841-55.
-
27Kumar D, Alvand A, Beacon JP. Impingement of infrapatellar fat pad (Hoffa’s disease): results of high-portal arthroscopic resection. Arthroscopy. 2007;23(11):1180-6.e1.
-
28Canale S, Beaty J. Campbell’s Operative Orthopaedics. Philadelphia, PA: Elsevier/Mosby; 2013.
-
29Indiran V, Jagannathan D. Osgood-Schlatter Disease. N Engl J Med. 2018;378(11):e15.
-
30Circi E, Atalay Y, Beyzadeoglu T. Treatment of Osgood-Schlatter disease: review of the literature. Musculoskelet Surg. 2017;101(3):195-200.
-
31Patel DR, Villalobos A. Evaluation and management of knee pain in young athletes: overuse injuries of the knee. Transl Pediatr. 2017;6(3):190-8.
-
32Arøen A, Løken S, Heir S, et al. Articular cartilage lesions in 993 consecutive knee arthroscopies. Am J Sports Med. 2004;32(1):211-5.
-
33Griffiths GP, Selesnick FH. Operative treatment and arthroscopic findings in chronic patellar tendinitis. Arthroscopy. 1998;14(8):836-9.
-
34Lam S, Amies V. Hip arthritis presenting as knee pain. BMJ Case Rep. 2015;2015:bcr2014208625.
-
35Tippett SR. Referred knee pain in a young athlete: a case study. J Orthop Sports Phys Ther. 1994;19(2):117-20.
-
36Castellet E, Vidal N, Conesa X. Escalas de valoración en cirugía ortopédica y traumatología. Trauma. 2010;21(1):34-43.
-
37Ware JE, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care. 1995;33(4 Suppl):AS264-279.
-
38Ashby E, Grocott MPW, Haddad FS. Outcome measures for orthopaedic interventions on the hip. J Bone Joint Surg Br. 2008;90(5):545-9.
-
39Alonso J, Prieto L, Antó JM. [The Spanish version of the SF-36 Health Survey (the SF-36 health questionnaire): an instrument for measuring clinical results]. Med Clin (Barc). 1995;104(20):771-6.
-
40Vilagut G, Valderas JM, Ferrer M, Garin O, López-García E, Alonso J. [Interpretation of SF-36 and SF-12 questionnaires in Spain: physical and mental components]. Med Clin (Barc). 2008;130(19):726-35.
-
41Hunt SM, McKenna SP, McEwen J, Williams J, Papp E. The Nottingham Health Profile: subjective health status and medical consultations. Soc Sci Med A. 1981;15(3 Pt 1):221-9.
-
42Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):53-72.
-
43Badia X, Roset M, Montserrat S, Herdman M, Segura A. [The Spanish version of EuroQol: a description and its applications. European Quality of Life scale]. Med Clin (Barc). 1999;112 Suppl 1:79-85.
-
44Vetrano M, Castorina A, Vulpiani MC, Baldini R, Pavan A, Ferretti A. Platelet-rich plasma versus focused shock waves in the treatment of jumper’s knee in athletes. Am J Sports Med. 2013;41(4):795-803.
-
45Hernández-Sánchez S, Hidalgo MD, Gómez A. Cross-cultural adaptation of VISA-P score for patellar tendinopathy in Spanish population. J Orthop Sports Phys Ther. 2011;41(8):581-91.
-
46Hárnandez-Sánchez S, Abat F, Hidalgo MD, et al. Confirmatory factor analysis of VISA-P scale and measurement invariance across sexes in athletes with patellar tendinopathy. J Sport Health Sci. 2017;6(3):365-71.
-
47Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011;63 Suppl 11:S240-52.
-
48De Vries AJ, van den Akker-Scheek I, Diercks RL, Zwerver J, van der Worp H. Effect of patellar strap and sports tape on jumper’s knee symptoms: protocol of a randomised controlled trial. J Physiother. 2013;59(4):270; discussion 270.
-
49Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop. 1985;(198):43-9.
-
50Abat F, Diesel WJ, Gelber PE, Polidori F, Monllau JC, Sánchez-Ibáñez JM. Effectiveness of the Intratissue Percutaneous Electrolysis (EPI®) technique and isoinertial eccentric exercise in the treatment of patellar tendinopathy at two years follow-up. Muscles Ligaments Tendons J. 2014;4(2):188-93.
-
51Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29(5):600-13.
-
52Rossi MJ, Lubowitz JH, Guttmann D. Development and validation of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2002;30(1):152.
-
53Hambly K, Griva K. IKDC or KOOS: which one captures symptoms and disabilities most important to patients who have undergone initial anterior cruciate ligament reconstruction? Am J Sports Med. 2010;38(7):1395-404.
-
54Arcuri F, Abalo E, Barcla F. Uso de escores para evaluación de resultados en cirugía del Ligamento Cruzado Anterior. Rev Artrosc Argent. 2010;17(3):241-7.
-
55Johnson DS, Smith RB. Outcome measurement in the ACL deficient knee--what’s the score? Knee. 2001;8(1):51-7.
-
56Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ; International Knee Documentation Committee. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006;34(1):128-35.
-
57Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159-63.
-
58Martínez-Cano J, Arango A, Castro A, Piña A, Martínez Rondanelli A. Validación de la Escala de Kujala para dolor patelofemoral en su versión en español. Rev CES Med. 2017;31(1):47-57.
-
59Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop. 1989;(248):13-4.
-
60Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN. The new Knee Society Knee Scoring System. Clin Orthop. 2012;470(1):3-19.
-
61Ares O, Castellet E, Maculé F, et al. Translation and validation of 'The Knee Society Clinical Rating System' into Spanish. Knee Surg Sports Traumatol Arthrosc. 2013;21(11):2618-24.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Don’t forget to remember
- Anatomical study on subtalar arthrodesis: anterolateral versus posterior portals
- Customized 3D printed guides for the repair of rupture of the posterior root of the internal meniscus. Preliminary outcomes
- Anatomical ligament reconstruction with allograft in chronic acromioclavicular dislocations restores joint stability and function. Short-term outcomes in 14 cases
- Patellar tendinopathy: diagnostic approach and functional assessment scales
- Current management of posterior cruciate ligament rupture. A narrative review
- Management of anterior instability of the shoulder with bone defects
- Open anatomical reconstruction surgical technique with allograft for the treatment of chronic acromioclavicular dislocations
- Simultaneous but different damage to both posterior meniscus roots with multiple ligament injury of the knee following high-energy trauma. Presentation of a case
- Pigmented villonodular synovitis of the ankle
Más en PUBMED
Más en Google Scholar


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.