Current management of posterior cruciate ligament rupture. A narrative review
Manejo actual de las roturas del ligamento cruzado posterior. Una revisión narrativa
Resumen:
El ligamento cruzado posterior (LCP) es el restrictor primario de la traslación posterior de la tibia y juega un papel fundamental en la estabilidad articular de la rodilla. Además de proveer una limitación para al desplazamiento posterior, el LCP también aporta estabilidad rotacional interna y externa a la rodilla. La edad media de la lesión es de 27 años, considerándose los accidentes de tráfico (45%) y las lesiones deportivas (40%) su principal etiología. Los mecanismos de producción primarios más comunes son el traumatismo directo sobre la tibial proximal con la rodilla flexionada a 90°, así como la hiperflexión e hiperextensión forzada de la rodilla. Las lesiones combinadas del LCP se suelen producir por mecanismos de varo y valgo forzados intensos que afectan a los estabilizadores primarios y secundarios de la rodilla. Las lesiones del LCP pueden identificarse en fase aguda, subaguda o crónica, siendo la exploración esencial para identificar lesiones asociadas. La radiografía simple y las pruebas de estrés permiten evaluar la gravedad de la lesión y son un buen complemento a la resonancia magnética, que es esencial en el diagnóstico. El patrón de lesión del LCP se divide en 3 tipos según su imagen en resonancia magnética: lesión parcial o intrasustancia, lesión completa y fractura avulsión en la inserción tibial. Se recomienda tratar de manera conservadora a pacientes con una lesión parcial aislada del LCP o con una lesión completa aislada que provoque solo una inestabilidad menor. Las indicaciones de tratamiento quirúrgico ante una lesión del LCP son: 1) fallos en el tratamiento conservador; 2) lesiones aisladas con traslaciones tibiales posteriores mayores de 1 cm; y 3) lesión del LCP en el contexto de una lesión multiligamentosa de rodilla.
Abstract:
The posterior cruciate ligament (PCL) is the primary restrictor of posterior translation of the tibia and plays a key role in knee joint stability. In addition to affording limitation of posterior displacement, the PCL also provides internal and external rotational stability of the knee. The mean patient age at PCL injury is 27 years, with traffic accidents (45%) and sports injuries (40%) being the leading causes. The most common primary causal mechanisms are direct proximal tibial trauma with the knee flexed 90º, as well as forced hyperextension and hyperflexion of the knee. Combined PCL injuries usually occur via intense forced varus and valgus mechanisms that affect the primary and secondary stabilizers of the knee. Posterior cruciate ligament injuries can be identified in the acute, subacute or chronic phase, with exploration being essential in order to detect associated lesions. Plain radiographs and stress tests allow us to evaluate the severity of the lesion, and are a good complement to magnetic resonance imaging (MRI), which is the key to diagnosis. Posterior cruciate ligament injuries are divided into three types according to their MRI characteristics: partial or intrasubstance lesions, complete lesions and avulsion fractures at the tibial insertion. Conservative management is advised in patients with isolated partial PCL injury or an isolated complete lesion causing only minor instability. Surgery in patients with PCL injury is indicated in the following situations: 1) failure of conservative management; 2) isolated lesions with posterior tibial translation >1 cm; and 3) PCL injury in the context of multiple ligament damage of the knee.
Introduction
Knowledge referred to the anatomy, biomechanics and treatment of the posterior cruciate ligament (PCL) has evolved in recent years, and the management tendencies have experienced changes as a result. Isolated PCL injuries are less common, typically occur simultaneous to rupture of the anterior cruciate ligament (ACL) or collateral ligaments, with a greater predominance among males, and are generally seen in the context of sports activities or traffic accidents.
The present narrative review analyses the most relevant practical aspects referred to the diagnosis of PCL rupture, and examines the different treatment options, establishing specific management recommendations based on the most recent literature. An exhaustive literature review was made to reach consensus on the key points regarding the diagnosis, treatment and rehabilitation of patients with PCL injuries. The review offers a comprehensive overview of PCL disease, ranging from the basic biomechanical and anatomical aspects to the different existing surgical and conservative management strategies.
Anatomy and biomechanics
The PCL receives its name from its posterior insertion in the tibia; it has broad femoral insertion (115 mm2) comprising the upper half of the medial surface of the medial femoral condyle, with its centre located about 7.9 mm from the distal joint cartilage (Figure 1), and it inserts in a bone depression of approximately 70 mm2 of surface area located between the two tibial plateaus and 5-10 mm below the posterior joint margin of the tibia. Previous studies have found the PCL to measure 30 mm in length on average, with a mean diameter of 11 mm. Its vascularization mainly comes from the middle genicular artery(1).
reacae.28373.fs2101003-figure1.png
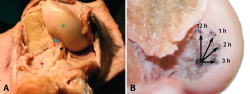
Figure 1. A: anatomical dissection of the posterior cruciate ligament (PCL)(blue asterisk), showing its femoral insertion in the medial femoral condyle (green asterisk), and its anterior relation to the anterior meniscofemoral ligament (black asterisk) and lateral meniscus (red asterisk); B: dissection of the femoral bone insertion of the PCL in the medial femoral condyle, together with a schematic representation of the clock dial coordinates system.
The PCL is related to the anterior and posterior meniscofemoral ligaments, which in turn receive their name from their relation to the PCL; at least one such ligament is found in 99% of all knees.
The PCL is the primary restrictor of posterior translation of the tibia and plays a key role in knee joint stability. The PCL is composed of two functionally distinguishable bundles: the large anterolateral (AL) bundle and the comparatively smaller posteromedial (PM) bundle. The activity of the AL bundle is fundamentally associated to flexion and that of the PM bundle to extension. However, it has been demonstrated that there is a gradual and synergic change in the tension-relaxation pattern of the two bundles over the range of motion of the knee, with both contributing to a certain degree. In addition to affording limitation of posterior displacement, the PCL also provides internal and external rotational stability of the knee(1).
Epidemiology and mechanism of injury
Injuries of the PCL have been traditionally underdiagnosed; as a result, it is difficult to establish their prevalence. Nevertheless, it has been estimated that such injuries may account for approximately 3% of all ligament lesions of the knee. The mean patient age at PCL injury is 27 years, with traffic accidents (45%) and sports injuries (40%) being considered the leading causes. Both isolated and combined injuries are more frequent in males, with rates of between 73-97%(2).
In order to establish a correct global diagnosis, it is important to take into account that concomitant lesions are usually also present - the most frequent being medial collateral ligament damage (42% of the cases), ACL lesions (12%) and chondral lesions in the lateral femorotibial compartment (32%). Only 5% of all the injuries occur isolatedly(3,4).
Damage to the PCL may result from both high- and low-energy traumatisms. High-energy trauma is predominantly associated with traffic accidents and contact sports. In traffic accidents, the lesion may be associated to fractures of the distal femur or proximal tibia(5).
The most frequent mechanisms of injury are: 1) direct trauma to the proximal tibia with the knee in 90° flexion. This is the most frequent scenario and is usually seen in traffic accidents in which the proximal extremity of the tibia impacts against the dashboard of the vehicle; 2) fall with forced hyperflexion of the knee, with the ankle in plantar flexion. This is the second most common mechanism and occurs as a result of trauma to the anterior tibial tuberosity, causing posterior displacement of the tibia over the femur. This is the most common mechanism in sports; and 3) forced hyperextension, associated with damage to the posterior capsule.
Combined PCL injuries usually occur via intense forced varus and valgus mechanisms that affect the primary and secondary stabilizers of the knee(6).
Diagnosis
Case history
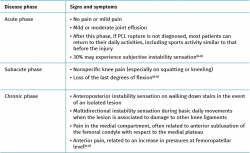
Isolated PCL injuries may go unnoticed for a number of reasons, in contrast to injuries of the ACL. Table 1(6,7,8) describes the signs and symptoms in the different stages of PCL injury.
With regard to gait disorders, patients may suffer limping in the early stages following the injury(9). Subsequently, in some cases, loss of restriction of external rotation of the tibia may give rise to gait with varus thrust or in hyperextension of the knee, which is noted in the support phase(9). Varus thrust is characterized by dynamic lateral inclination during the support phase, which produces increased loading in the medial compartment. Other patients may walk with a knee slightly flexed in order to avoid the pain and instability associated to varus thrust(9). These gait patterns are usually more often seen in combined injuries affecting the posterolateral complex (PLC), in the same way as varus axis alteration(9).
Physical examination
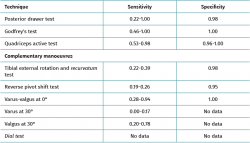
Some exploratory manoeuvres are specific of PCL injury, while others indicate associated lesions. Their sensitivity and specificity are reported in Table 2. Bilateral manoeuvring is recommended in all cases, involving both knees, in order to distinguish between physiological hyperlaxity and pathological instability.
• Posterior drawer test. This is done with the patient in supine decubitus and the knee in 90° flexion. The test involves the application of pressure in a posterior direction of the proximal region of the tibia, observing posterior tibial translation in the injured knee with respect to the contralateral knee (Figure 2). A posterior displacement of the tibia of 0-5 mm is considered to correspond to a grade I lesion, 6-10 mm to a grade II lesion and >10 mm to a grade III lesion. Assessment of the degree of displacement is subjective, and thus implies important interobserver variability. If the tibial plateau remains located anterior to the medial femoral condyle, the lesion is considered to correspond to grade I, while if it is located at the same level as the femoral condyle the lesion corresponds to grade II, and if the plateau extends beyond the medial femoral condyle, the lesion corresponds to grade III (Figure 2)(10,11).
• Godfrey's test (posterior sag sign). This test evaluates posterior tibial translation, placing the patient in supine decubitus with both knees and hips flexed 90°. The examiner places his or her arm beneath both Achilles tendons, leaving the tibias of the patient hanging. If the PCL is damaged, erasure/collapse of the anterior tibial tuberosity can be seen in a lateral view, particularly when compared with the healthy knee (Figure 3)(10,11).
• Quadriceps active test. This test is performed with the patient knee in 90° flexion and the foot resting on the exploration table. The patient is instructed to try to slide the foot forward while keeping it blocked, which induces isometric contraction of the quadriceps muscle. Anterior tibial translation of at least 2 mm with this test is suggestive of damage to the PCL(10,11).
As has been mentioned above, patients with posterior instability of the knee often suffer concomitant lesions, including damage to the MCL and the PLC. It is therefore advisable to perform complementary exploratory manoeuvres to detect these possible concomitant lesions:
• Tibial external rotation and recurvatum test. This test may indicate combined injury of the ACL or PCL together with the PLC. The examiner may detect the position in varus, recurvatum and external rotation of the tibia, raising the legs in extension and holding only the big toe. A difference between the two legs suggests damage to the PLC(10,11).
• Reverse pivot shift test. This test is made with the patient in supine decubitus, the knee in 90° flexion and the foot in external rotation. The examiner applies force in valgus and at the same time extends the knee, noting how the lateral tibial plateau reduces from its posterior subluxation position in cases of combined injuries of the PCL and PLC(10,11).
• Dial test. This manoeuvre evaluates rotational instability. With the patient in prone decubitus, external tibial rotation is measured in 30° and 90° flexion of the knee; a difference of over 10° between the tested knee and the healthy knee is considered to be pathological. Asymmetry only observed at 30° of flexion is suggestive of an isolated PLC lesion, while asymmetry observed at 30° and 90° should cause us to suspect combined injury of the PCL and PLC (Figure 4). Although the diagnostic precision of this test is questioned, it has been biomechanically validated for assessing the severity of posterolateral lesions of the knee(10,11).
Imaging diagnosis
Imaging studies in patients with PCL injuries are important in order to quantify instability, since clinical evaluation alone may prove scantly reliable in distinguishing the degree of displacement of the tibia with respect to the femur.
Plain radiographs
Although the soft tissues are not visualized on the plain radiographs, the behaviour of the bone elements provides indirect information on damage to the PCL or the presence of associated lesions. Simple anteroposterior (AP) and lateral views can be used to evaluate fractures or avulsions (arcuate sign) of the head of the fibula or the femoral condyles, or tibial bone avulsions.
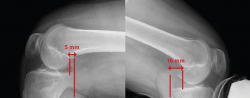
Stress radiography
Comparative stress radiographs play an important role, since they allow us to quantify and visualize posterior tibial sag in PCL injuries and assess possible associated sagittal instabilities(12,13).
• Hamstring contraction view: this is obtained with the patient seated and the knee flexed 90°. While the patient is instructed to perform maximum ischiotibial (hamstring) contraction against resistance placed at the level of the calcaneus, a strict lateral view of the knee is obtained. By comparing the profile of both knees, we can determine whether ischiotibial contraction causes posterior displacement of the tibia(12,13).
• Kneeling view: the patient kneels down on a platform reaching the anterior tibial tuberosity. The knees are to be in 90° flexion and the hips in 180°. A strict lateral view is obtained of both knees, evaluating the difference in posterior tibial translation. This view simulates quantification of the posterior drawer test, and is the easiest view to obtain and also the most widely used in clinical practice(12,13).
• Telos® system: this system allows us to apply constant and quantifiable force to the knee in different planes. If we wish to evaluate the PCL, the force is exerted on the anterior tibial tuberosity with the knee flexed 90°. A strict lateral view is obtained of both knees, evaluating the difference in posterior tibial translation(12,13).
The classification of PCL injuries according to the observed posterior translation is as follows:
– Partial injury of the PCL if there is an increase in posterior translation of <8 mm.
– Isolated complete injury if translation is between 8-12 mm.
– Injury of the PCL with other associated lesions (posterolateral or posteromedial) if there is >12 mm of posterior translation.
Posterior translation of the tibia is measured as the minimum distance between a line tangential to the posterior cortical layer of the tibia and another line tangential to the posterior margin of the femoral condyle at the most dorsal point of the Blumensaat line (Figure 5)(12,13).
Magnetic resonance imaging
Although the diagnosis of PCL rupture is essentially clinical, and instability is quantified from stress radiographs, magnetic resonance imaging (MRI) is the technique of choice for the diagnosis and follow-up of PCL lesions subjected to conservative management, and affords excellent information on the presence of associated injuries - not only ligament damage but also meniscal or chondral lesions. In addition, MRI is able to distinguish between acute and chronic injuries, since the absence of soft tissue edema and of bone contusion (usually affecting the anterior portion of the tibia) is indicative of a chronic lesion(13,14).
Posterior cruciate ligament injuries are divided into three types according to their MRI characteristics: partial or intrasubstance lesions (Figure 6A), complete lesions (Figure 6B) and avulsion fractures at the tibial insertion (Figure 6C)(13,14). Most complete lesions occur in the middle portion of the ligament, which is not correctly visualized in the axial and coronal planes; the gold standard therefore is evaluation of images in the sagittal plane(13,14).
reacae.28373.fs2101003-figure6.png
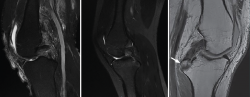
Figure 6. A: magnetic resonance imaging (MRI) sagittal view in T2-weighted sequencing, showing partial rupture; B: complete rupture of the posterior cruciate ligament (PCL); C: MRI sagittal view in T1-weighted sequencing of the left knee. The white arrow indicates avulsion of the PCL with a bone fragment in the tibial insertion.
Treatment
Conservative management
Posterior cruciate ligament injuries often occur as part of a multiple ligament lesion of the knee, though isolated presentations are sometimes observed. Conservative management of isolated injuries of the PCL has shown good outcomes due to the intrinsic healing capacity of the PCL and the good functional compensation which the quadriceps muscle can provide in a knee in the absence of the PCL(15). Thus, conservative management is advised in patients with isolated partial PCL injury or an isolated complete lesion causing only minor instability(16).
However, PCL deficiency results in altered knee kinematics and loads, giving rise to a prevalence of moderate to severe osteoarthrosis of approximately 10% over the long term(17). Consequently, patients should always be informed that conservative management does not result in healing, and that in the case of objective moderate to severe instability, symptoms of instability or pain may develop in relation to cartilage disorders over time, even if initially no symptoms are experienced and the lesion does not prevent the patient from returning to his or her daily activity - including sports(18).
Conservative management should include the use of knee pads to prevent posterior tibial subluxation, thanks to pressure mechanisms located in the posterior part of the upper third of the tibia. This measure reduces the risk of ligament healing occurring in a non-anatomical position, and minimizes the likelihood of a certain degree of residual laxity. These knee pads are defined as "dynamic" (Figure 7), as they vary the pressures exerted during flexion-extension, since tension in the PCL is not constant and proves greater at 45° of flexion(19,20).
In addition to the use of specific knee pads for the PCL, during the first two months it is advisable to prescribe reinforcement of the quadriceps muscle (agonist of the PCL) and avoid ischiotibial exercises (antagonists of the PCL) that can increase posterior tibial translation, causing additional stress over the PCL in its healing process(20).
Surgical treatment
Surgery in patients with PCL injury is indicated in the following situations: 1) failure of conservative management (persistence of instability associated to pain after 6 months with adequate conservative management); 2) isolated lesions with posterior tibial translation >1 cm; and 3) PCL injury in the context of multiple ligament damage of the knee. Although these indications are universally accepted, to date no long-term studies have been able to demonstrate that reconstruction of the PCL serves to prevent the development of gonarthrosis, even if it reduces the related symptoms. This is probably due in part to the inconsistent efficacy of reconstruction of this ligament in restoring normal knee function and kinematics - the most frequently reported complication being residual laxity(19).
Classification of the PCL injuries into different patterns can guide management, since fracture-avulsion may be surgically treated through anchoring of the bone fragment, and substance lesions are amenable to intraligamentous augmentation in the acute phase, while a partial lesion can be a candidate for conservative management. Lastly, complete rupture at the femoral insertion can only be treated through complete reconstruction of the ligament if clinical evaluation detects significant instability(21).
The best or most effective technique for PCL reconstruction remains the subject of debate. Different procedures have been described according to the tibial fixation involved (transtibial or inlay), reconstruction of the PM and/or AL bundles (simple or double), according to the femoral tunnelling technique used (inside-out or outside-in), the type of fixation (interferential screws, pressure adjustment, fixed or adjustable loop), and the type of graft employed. With regard to the type of graft, utilization of patellar, quadricipital and even ischiotibial tendon has been described, whether autologous or from tissue banks (allograft)(21). The inlay technique is the only procedure requiring an open PM approach to reach the anatomical point of insertion of the PCL, with the purpose of preparing a trench for fixing a bone block of the new graft. Since the current arthroscopic techniques have demonstrated optimum outcomes, nowadays the inlay technique is reserved only for complex revision surgery or in cases of ligament lesions associated to fractures of the tibial plateau(22).
Arthroscopic portals
Depending on the preferences and experience of the surgeon, reconstruction of the PCL can be made through different portals. The standard anteromedial and anterolateral portals are routinely used for joint revision surgery and the treatment of associated chondral, ligamentous or meniscal lesions. Some authors use posteromedial and posterolateral portals to adopt a trans-septal approach (Kim's technique) and thus work exclusively from the back of the knee. Other surgeons prefer a portal through the patellar tendon (Gillquist portal) in combination with a posteromedial portal, alternating them as viewing and working portal. Utilization of the transpatellar portal is simpler in the case of combined rupture of the ACL and PCL, since the intercondylar space is completely vacant (Figure 8)(23).
reacae.28373.fs2101003-figure8.png
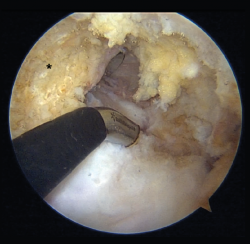
Figure 8. "Vacant" intercondylar space in combined rupture of the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL) in a left knee. The surgeon is using the transpatellar (Gillquist) portal for viewing and the anteromedial portal for working with radiofrequency. The working cannula placed in a posteromedial portal can also be seen. The black asterisk indicates the lateral wall of the medial femoral condyle, as the femoral insertion site of the PCL.
In the case of isolated PCL rupture, 70° optics instead of the conventional 30° optics can be used to obtain a wider view from the anterior portals. Lastly, a reconstruction technique has been described that only uses the anterolateral viewing portal (through the intercondylar space with 70° optics) and the anteromedial working port - with no need for posterior portals. This latter technique requires specifically designed instruments, however; as a result, it is not widely used(23,24,25).
Tibial tunnel
The tibial tunnel is regarded as the most complex part of the operation; firstly, due to the risk of vascular damage on creating the tunnel, and secondly because it is not always easy to reach the original PCL insertion site(26).
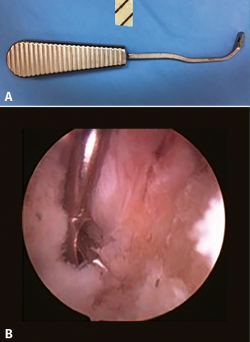
The tunnel can be made medial or lateral to the anterior tibial tuberosity. If the tunnel is created from the anteromedial zone, it will be oriented directly towards the neurovascular structures of the posterior part of the knee - thus increasing the risk of complications. Furthermore, even if the tunnel ends at the anatomical insertion site, its orientation increases the difficulty of advancing the plasty because of the so-called killer turn, i.e., the very marked angle which the plasty must follow until it is positioned in the femoral tunnel. Performing the tunnel from the anterolateral part of the tibia lowers the risk of neurovascular damage and reduces the killer turn(26). Good control is important in this phase, due to the risk of vascular damage on emerging from the tibial tunnel. Some authors prefer to arthroscopically visualize emergence from the tunnel and place a specifically shaped metal protector (Figure 9) to avoid abrupt emergence. Other authors prefer fluoroscopic control of emergence from the tunnel.
The anatomical references for arthroscopically recognizing the tibial insertion site of the PCL are the most posterior and lateral fibers of the posterior horn of the medial meniscus (Figure 10), defined as shining white fibers that delimit the insertion site medially, and the fibers of the popliteus muscle that indicate the distal margin (27).
reacae.28373.fs2101003-figure10.png
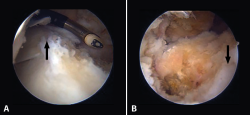
Figure 10. A: view from a transpatellar (Gillquist) portal. From the posteromedial working portal we use radiofrequency to clean the tibial insertion site of the posterior cruciate ligament (PCL) which is located in the posterolateral zone of the posterior root of the medial meniscus (arrow); B: view from a posteromedial portal. Fully cleaned tibial insertion site with the arrow indicating the posterior root of the medial meniscus.
By using fluoroscopy, and in addition to allowing controlled emergence in the posterior part of the knee, we can radiologically confirm that emergence from the tunnel is perfectly anatomical. In lateral view, the tunnel should emerge approximately 7 mm proximal to the so-called champagne-glass drop-off, and in anteroposterior view at the medial margin of the lateral tibial spine, 2 mm distal to the joint line. Likewise, regardless of whether a double or simple bundle technique is used, only one tibial tunnel is made that can be complete or partial with a retrograde guide according to the preferred fixation technique at tibial level(27).
Femoral tunnel
Two anatomical references have been described that indicate the location of the insertions of the two PCL bundles in the femur: the most distal point of the centre of the trochlear groove (the trochlear point) and the midpoint of the intercondylar arch at internal femoral condylar level (the medial arch point), delimiting the AL bundle that ends its distal insertion precisely at subchondral level. The PM bundle in turn is located more dorsal and proximal to that point (about 10 mm from the chondral margin)(27).
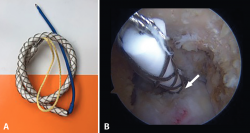
In the case of single bundle reconstructions, we should seek to position the tunnel at the centre of the two original insertion sites, with a slight tendency to reproduce the AL bundle, which is anatomically more consistent and mechanically more resistant. In the case of double bundle reconstructions, the originally described technique contemplates an 11-mm tunnel at the level of the AL bundle insertion site and a 7-mm tunnel at the PM bundle insertion site, leaving a minimum 2-mm bone bridge between the two of them (Figure 11)(28).
reacae.28373.fs2101003-figure11.png
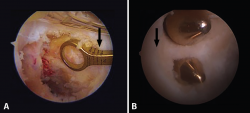
Figure 11. A: single bundle reconstruction. The outside-in drilling guide indicates how many millimetres the femoral tunnel is being positioned from the chondral margin (arrow); B: double bundle reconstruction. Note the distance from the chondral margin (arrow) and the bone bridge between the two tunnels.
In the case of double bundle reconstructions, it is advisable to use an inside-out technique from the anterolateral portal for drilling of the tunnels, since an outside-in tunnel could more easily cause collision if specific guides are not used. In order to position the tunnel of the AL bundle as distal as possible without damaging the cartilage, it is advisable to advance the cannulated drill through the anterolateral portal, positioning it where drilling is required, and then advance the guide needle through the drill to fix the direction.
In the case of single bundle reconstructions, both inside-out and outside-in drilling can be used. The latter technique allows the tunnel to be performed more distal, reducing the risk of cartilage damage, since the direction of the tunnel will be divergent with respect to the joint surface. Depending on the preferred type of femoral fixation, a complete or partial outside-in tunnel can be made with a retrograde guide drill(29,30).
Plasty tunnelling and fixation
If a complete tibial tunnel has been made, and in order to facilitate plasty placement, it is advisable to position metal dilators in the tunnel, together with the use of a so-called smoother. The latter is a band covered by a metal mesh. On advancing through the tunnel, it smoothens the walls and the edges at the entrance and exit of the tunnel. This facilitates plasty placement on emerging from the tunnel, and avoids damage caused by friction with the tunnel margins, partially reducing the aforementioned killer turn (Figure 12)(30,31).
If patellar tendon is used, positioning of the bone block may be more complex than when soft tissue is employed, since the lack of space in the posterior compartment and the stiffness of the bone block used in the patellar tendon do not allow easy movement. In these cases it is advisable to divide the block transversely into two parts, keeping the periosteum of the distal surface of the bone block intact so that the two parts stay together. In this way the bone block can be passed more easily, since it can be doubled into two at the exit from the tibial tunnel. In the double bundle technique it is common to use Achilles tendon for the AL bundle and anterior tibial tendon for the PM bundle (both from the tissue bank), through one same tibial tunnel(31).
The femur is usually fixed first and then the tibia, performing an anterior drawer at 90° flexion. In the case of double bundle reconstructions and the use of an interference screw as fixation method in the femur, it is advisable to place the PM screw in the posterior and lower part of the tunnel, while the AL screw should be placed in an anterosuperior position. Only in the case of all-inside reconstructions using two adjustable fixations and two partial tunnels do we perform combined tensioning of both fixation systems. For the tibial fixation of a double bundle, the AL is fixed first, performing an anterior drawer at 90° with the foot in neutral rotation. We then fix the PM bundle with the knee in full extension. Fixation is usually made using cortical screws with a washer or staples(31).
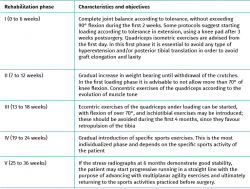
Rehabilitation and return to sports activity
Although different rehabilitation programs are available, there are key elements that should establish the basis of any protocol. These elements include initial limitation of weight bearing, the prevention of posterior tibial subluxation, and early strengthening of the quadriceps muscle. With regard to loading, the described protocols are highly variable, with a minimum period of avoidance of weight bearing of between 3-6 months, since it has been demonstrated that PCL graft healing takes almost twice as long as ACL graft healing(32,33). In the immediate postoperative period, simple immobilization in extension is required during the first 72 hours to avoid high pressures in edematous zones of the operated knee. After this period we can switch to a dynamic knee pad specific for the PCL that continuously maintains a certain anterior drawer through the application of sustained pressure in the posterior zone of the tibia. It is advisable to wear these knee pads 24 hours a day for at least 2-3 months. Some rehabilitation protocols even extend this period to 6 months after surgery(32,33). A progressive postoperative rehabilitation program is indicated, with clear objectives and divided into 5 phases, that has been shown to be the best strategy for securing improved stabilization of posterior tibial translation, varus and external rotation (Table 3)(4).
Most patients return to sports activity between 9-12 months after the operation, depending on their clinical course and only if the required criteria are met: adequate neuromuscular control in activities over different types of terrain, with no evidence of instability, pain or inflammation(32,33).
Conclusions
The management of PCL rupture has changed in recent years, with a growing tendency to reconstruct the ligament. Advances in knowledge referred to anatomy and biomechanics, and clinical follow-up studies, have led to a renovation of the surgical reconstruction techniques and rehabilitation protocols. In well selected cases, the surgical outcomes are very good. The present review offers an update on all the clinical and surgical aspects to be considered in the management of PCL rupture.
Figuras
Figure 1. A: anatomical dissection of the posterior cruciate ligament (PCL)(blue asterisk), showing its femoral insertion in the medial femoral condyle (green asterisk), and its anterior relation to the anterior meniscofemoral ligament (black asterisk) and lateral meniscus (red asterisk); B: dissection of the femoral bone insertion of the PCL in the medial femoral condyle, together with a schematic representation of the clock dial coordinates system.
Figure 2. Initial position of the tibia reduced in the posterior drawer manoeuvre (A) compared with posterior tibial translation without reduction (B).
Figure 3. Godfrey's test, showing the difference between posterior translation of the tibia in a right knee with posterior cruciate ligament (PCL) injury versus the healthy left knee.
Figure 4. The dial test, showing the difference in external rotation at 90° between the right knee with damage to the posterior cruciate ligament (PCL) and posterolateral complex (PLC) versus the healthy left knee.
Figure 5. Telos system. The red line indicates measurement of posterior translation of the tibia: the difference between the healthy right knee and the left knee is 11 mm in this case - suggestive of isolated complete posterior cruciate ligament (PCL) rupture.
Figure 6. A: magnetic resonance imaging (MRI) sagittal view in T2-weighted sequencing, showing partial rupture; B: complete rupture of the posterior cruciate ligament (PCL); C: MRI sagittal view in T1-weighted sequencing of the left knee. The white arrow indicates avulsion of the PCL with a bone fragment in the tibial insertion.
Figure 7. Dynamic knee pad for the posterior cruciate ligament (PCL), with variable pressure mechanism at the posterior part of the proximal third of the tibia.
Figure 8. "Vacant" intercondylar space in combined rupture of the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL) in a left knee. The surgeon is using the transpatellar (Gillquist) portal for viewing and the anteromedial portal for working with radiofrequency. The working cannula placed in a posteromedial portal can also be seen. The black asterisk indicates the lateral wall of the medial femoral condyle, as the femoral insertion site of the PCL.
Figure 9. A: example of protector for exit from the tibial tunnel of the posterior cruciate ligament (PCL); B: the protector prevents progression of the guide needle towards the soft tissues of the posterior region of the knee.
Figure 10. A: view from a transpatellar (Gillquist) portal. From the posteromedial working portal we use radiofrequency to clean the tibial insertion site of the posterior cruciate ligament (PCL) which is located in the posterolateral zone of the posterior root of the medial meniscus (arrow); B: view from a posteromedial portal. Fully cleaned tibial insertion site with the arrow indicating the posterior root of the medial meniscus.
Figure 11. A: single bundle reconstruction. The outside-in drilling guide indicates how many millimetres the femoral tunnel is being positioned from the chondral margin (arrow); B: double bundle reconstruction. Note the distance from the chondral margin (arrow) and the bone bridge between the two tunnels.
Figure 12. Smoother (A) used to minimize the killer turn (B) at exit from the tibial tunnel (white arrow).
Tablas
Table 1. Patient signs and symptoms during the different phases of posterior cruciate ligament (PCL) injuries
Table 2. Sensitivity and specificity of the exploratory manoeuvres in isolated posterior cruciate ligament (PCL) injuries
Información del artículo
Cita bibliográfica
Autores
Simone Perelli Perelli
Institut Català de Traumatologia i Medicina de l'Esport (ICATME). Hospital Universitari Dexeus. Universitat Autònoma de Barcelona (UAB)
Parc de Salut Mar. Barcelona
Ángel Masferrer-Pino
Institut Català de Traumatologia i Medicina de l'Esport (ICATME). Hospital Universitari Dexeus. Universitat Autònoma de Barcelona (UAB)
Rodolfo Morales Avalos
Unidad de Rodilla. Hospital Universitari Dexeus. Institut Català de Traumatologia i Medicina de l’Esport (ICATME). Universitat Autònoma de Barcelona
Servicio de Ortopedia y Traumatología. Hospital Universitario. Universidad Autónoma de Nuevo León. Monterrey. NL, México
David Barastegui Fernández
Instituto Cugat-Hospital Quirónsalud Barcelona
Mutualidad de Futbolistas Españoles. Delegación de Cataluña. Barcelona
Servicio de Cirugía Ortopédica, Artroscopia y Traumatología Deportiva. Instituto Cugat. Barcelona
Mutualitat Catalana de Futbolistes. Federació Catalana de Futbol. Real Federación Española de Fútbol
ITQB. Hospital Quirónsalud Barcelona
Universitat Internacional de Catalunya. Sant Cugat del Vallès
Fundación García Cugat. Cátedra de la Universidad CEU Cardenal Herrera. Valencia
Alfonso Espinosa Ruiz
Hospital Quirónsalud Ciudad Real
Javier Tejada Gallego
Departamento de Cirugía Ortopédica y Traumatología. Clínica Universidad de Navarra. Madrid
Raphael Idiart
Hospital Vithas Xanit de Benalmádena. Hospital CHIP Málaga. Instituto Malagueño de Traumatología y Medicina del Deporte (IMATDE)
Álvaro Acebrón Fabregat
Servicio de Traumatología y Cirugía Ortopédica. Hospital Clínico Universitario de Valencia
Servicio de Ortopedia y Traumatología. Unión de Mutuas. Valencia
Nuria Urquiza Alcaraz
Hospital Universitario de Donostia. Guipuzkoa
Hospital Quirónsalud Bizkaia
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved experiments in humans or in animals.
Data confidentiality. The authors declare that the protocols of their centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Young Arthroscopy Group (Grupo Joven de Artroscopia [GJA])
This study has been coordinated and carried out within the context of the Young Arthroscopy Group (Grupo Joven de Artroscopia [GJA]) project of the Spanish Association of Arthroscopy (Asociación Española de Artroscopia [AEA]).
Referencias bibliográficas
-
1Ahmad CS, Cohen ZA, Levine WN, Gardner TR, Ateshian GA, Mow VC. Codominance of the individual posterior cruciate ligament bundles. An analysis of bundle lengths and orientation. Am J Sports Med. 2003;31(2):221-5.
-
2Schulz MS, Russe K, Weiler A, Eichhorn HJ, Strobel MJ. Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg. 2003;123(4):186-91.
-
3Logan CA, Beaulieu-Jones BR, Sánchez G, et al. Posterior cruciate ligament injuries of the knee at the National Football League Combine: an imaging and epidemiology study. Arthroscopy. 2018;34(3):681-6.
-
4LaPrade CM, Civitarese DM, Rasmussen MT, LaPrade RF. Emerging Updates on the Posterior Cruciate Ligament: A Review of the Current Literature. Am J Sports Med. 2015;43(12):3077-92.
-
5López-Vidriero E, Simon DA, Johnson DH. Initial evaluation of posterior cruciate ligament injuries: history, physical examination, imaging studies, surgical and nonsurgial indications. Sports Med Arthrosc. 2010;18:230.
-
6Margheritini F, Mariani PP. Diagnostic evaluation of posterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2003;11(5):282-8.
-
7McAllister DR, Petrigliano FA. Diagnosis and treatment of posterior cruciate ligament injuries. Curr Sports Med Rep. 2007;6:293.
-
8Bedi A, Musahl V, Cowan JB, Management of Posterior Cruciate Ligament Injuries: An Evidence-Based Review. J Am Acad Orthop Surg. 2016;24:277-89.
-
9Harner CD, Höher J. Evaluation and treatment of posterior cruciate ligament injuries. Am J Sports Med. 1998;26(3):471.
-
10Wind WM Jr, Bergfeld JA, Parker RD. Evaluation and treatment of posterior cruciate ligament injuries: revisited. Am J Sports Med. 2004;32(7):1765.
-
11Kopkow C, Freiberg A, Kirschner S, Seidler A, Schmitt J. Physical examination tests for the diagnosis of posterior cruciate ligament rupture: a systematic review. J Orthop Sports Phys Ther. 2013;43(11):804-13.
-
12Jung TM, Reinhardt C, Scheffler SU, Weiler A. Stress radiography to measure posterior cruciate ligament insufficiency: a comparison of five different techniques. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1116-21.
-
13Mariani PP, Margheritini F, Christel P, Bellelli A. Evaluation of posterior cruciate ligament healing: a study using magnetic resonance imaging and stress radiography. Arthroscopy. 2005;21(11):1354-61.
-
14Sonin AH, Fitzgerald SW, Friedman H, Hoff FL, Hendrix RW, Rogers LF. Posterior cruciate ligament injury: MR imaging diagnosis and patterns of injury. Radiology. 1994;190(2):455-8.
-
15Shelbourne KD, Clark M, Gray T. Minimum 10-year follow-up of patients after an acute, isolated posterior cruciate ligament injury treated nonoperatively. Am J Sports Med. 2013;41(7):1526-33.
-
16Parolie JM, Bergfeld JA. Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med. 1986;14(1):e35-8.
-
17Geissler WB, Whipple TL. Intraarticular abnormalities in association with posterior cruciate ligament injuries. Am J Sports Med. 1993;21(6):e846-849.
-
18Shelbourne KD, Davis TJ, Patel DV. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries. A prospective study. Am J Sports Med. 1999;27(3):e276-83.
-
19Boynton MD, Tietjens BR. Long-term followup of the untreated isolated posterior cruciate ligament-deficient knee. Am J Sports Med. 1996;24(3):e306-10.
-
20Agolley D, Gabr A, Benjamin-Laing H, Haddad FS. Successful return to sports in athletes following non-operative management of acute isolated posterior cruciate ligament injuries: medium-term follow-up. Bone Joint J. 2017;99-B(6):774-8.
-
21Johnson P, Mitchell SM, Görtz S. Graft Considerations in Posterior Cruciate Ligament Reconstruction. Curr Rev Musculoskelet Med. 2018;11(3):521-7.
-
22Stannard JP. Tibial Inlay Posterior Cruciate Ligament Reconstruction. Sports Med Arthrosc Rev. 2020;28(1):14-7.
-
23Lee DW, Choi HW, Kim JG. Arthroscopic Posterior Cruciate Ligament Reconstruction With Remnant Preservation Using a Posterior Transeptal Portal. Arthrosc Tech. 2017;6(5):e1465-e1469.
-
24Chen T, Liu S, Chen J. All-Anterior Approach for Arthroscopic Posterior Cruciate Ligament Reconstruction With Remnant Preservation. Arthrosc Tech. 2016;5(6):e1203-e1207.
-
25Nancoo TJ, Lord B, Yasen SK, Smith JO, Risebury MJ, Wilson AJ. Trans Medial All-Inside Posterior Cruciate Ligament Reconstruction Using a reinforced Tibial Inlay Graft. Arthrosc Tech. 2013;2(4):e381-8.
-
26Kim SJ, Shin JW, Lee CH, et al. Biomechanical Comparison of Three Different Tibial Tunnel Directions in Posterior Cruciate Ligament Reconstruction. Arthroscopy. 2005;21(3):286-93.
-
27Lee DY, Kim DH, Park JS, et al. Systematic Review of Cadaveric Studies on Anatomic Posterior Cruciate Ligament Reconstruction: the Landmarks in Anatomic Posterior Cruciate Ligament Reconstruction. Knee Surg Relat Res. 2014;26(4):191-8.
-
28Lee DY, Kim DH, Kim HJ, Nam DC, Park JS, Hwang SC. Biomechanical Comparison of Single-Bundle and Double-Bundle Posterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. JBJS Rev. 2017;5(10):e6.
-
29Kim JH, Kim HY, Lee DH. Location of the Femoral Tunnel Aperture During Single-Bundle Posterior Cruciate Ligament Reconstruction: Outside-In Versus Inside-Out Techniques. Int Orthop. 2018;42(9):2097-103.
-
30Spiridonov SI, Slinkard NJ, LaPrade RF. Isolated and combined grade-III posterior cruciate ligament tears treated with double-bundle reconstruction with use of endoscopically placed femoral tunnels and grafts: operative technique and clinical outcomes. J Bone Joint Surg Am. 2011;93(19):1773-80.
-
31Kim SJ, Kim TE, Jo SB, Kung YP. Comparison of the Clinical Results of Three Posterior Cruciate Ligament Reconstruction Techniques. J Bone Joint Surg Am. 2009;91(11):2543-9.
-
32Wang D, Graziano J, Williams RJ 3rd, Jones KJ. Nonoperative Treatment of PCL Injuries: Goals of Rehabilitation and the Natural History of Conservative Care. Curr Rev Musculoskelet Med. 2018;11(2):290-7.
-
33Kim JG, Lee YS, Yang BS, Oh SJ, Yang SJ. Rehabilitation After Posterior Cruciate Ligament Reconstruction: A Review of the Literature and Theoretical Support Arch Orthop Trauma Surg. 2013;133(12):1687-95.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Don’t forget to remember
- Anatomical study on subtalar arthrodesis: anterolateral versus posterior portals
- Customized 3D printed guides for the repair of rupture of the posterior root of the internal meniscus. Preliminary outcomes
- Anatomical ligament reconstruction with allograft in chronic acromioclavicular dislocations restores joint stability and function. Short-term outcomes in 14 cases
- Patellar tendinopathy: diagnostic approach and functional assessment scales
- Current management of posterior cruciate ligament rupture. A narrative review
- Management of anterior instability of the shoulder with bone defects
- Open anatomical reconstruction surgical technique with allograft for the treatment of chronic acromioclavicular dislocations
- Simultaneous but different damage to both posterior meniscus roots with multiple ligament injury of the knee following high-energy trauma. Presentation of a case
- Pigmented villonodular synovitis of the ankle
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.