Introduction
The meniscal roots are essential for preventing meniscal extrusion and for transforming axial loading into circumferential loading at intraarticular level within the knee(1,2,3). Root tearing is defined as avulsion damage to the meniscotibial ligament (ligament of the root) on the tibial plateau or as radial tearing of the meniscus within the first centimetre of its insertion in the bone(4,5). This type of meniscal damage most often affects the posterior roots(3). Tearing of the external posterior root is usually caused by trauma and is seen in 7-12% of all patients with tearing of the anterior cruciate ligament (ACL)(6). Lesions of the internal posterior root are mainly a consequence of chronic meniscal degenerative processes in middle aged and typically female individuals, representing up to 10-28% of the lesions subjected to arthroscopic surgery. In this regard, trauma induced damage to the internal roots is less frequent, though it has been reported in patients with multiple ligament lesions(6).
The most widely accepted classification of the different types of lesions is that proposed by LaPrade, which divides rupture injuries into 5 types according to their morphological characteristics(7), and moreover specifies the frequency of each of them:
- Type 1 (7%): partial and stable rupture of the posterior root.
- Type 2 (67%): complete radial rupture in the 9 mm proximal to the bone insertion. Type 2A (38%): at less than 3 mm; type 2B (16.9%): between 3 and < 6 mm; type 2C (12.7%): 6-9 mm.
- Type 3 (6%): bucket handle meniscus rupture with complete deinsertion of the meniscal root.
- Type 4 (10%): longitudinal or complete oblique rupture with complete deinsertion of the meniscal root.
- Type 5 (10%): bone avulsion of the insertion of the meniscal root.
Bone avulsion of the root in the internal meniscus (type 5) is very rare(2,3,5). Our review of the literature only revealed a single reported case of simultaneous traumatic injury of both posterior roots(8), without involvement of the ligaments.
Clinical case
We present the case of a 30-year-old male seen in the emergency room of our hospital as a consequence of a motorcycle accident. Initial clinical evaluation revealed important hemarthrosis of the knee, with pain in response to palpation of the medial joint line and of the external tibial plateau, with limitation of joint balance control. The stability tests were masked by the pain; however, the posterior drawer test proved negative, while the Lachman test was positive. The collateral ligaments presented stability without laxity. Vascular or neurological damage was discarded by the sensory-motor exploration and the palpation of distal pulses.
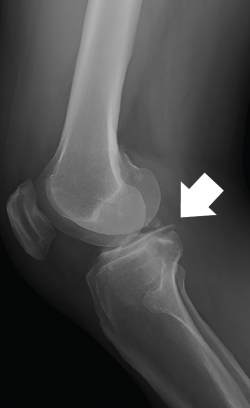
The plain radiographs revealed bone avulsions of the posterior part of the tibia (Figure 1).
The computed tomography (CT) study evidenced a fracture of the posterior region of the internal tibial plateau with millimetric collapse and sub-centimetre avulsed fragments located immediately medial to the posterior cruciate ligament (PCL), together with a small fracture in the posterior cortical layer of the external tibial plateau without collapse, displacement or comminution (Figure 2).
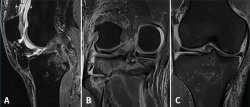
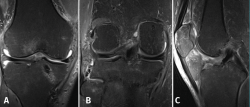
Magnetic resonance imaging (MRI) revealed multiple contusion edema zones with severe partial rupture of the ACL and grade I-II lesion of the PCL, with normal insertion at distal level (Figure 3A). In addition, proximal distension of the medial collateral ligament (MCL) and lateral collateral ligament (LCL) was observed, together with damage to the external meniscus posterior root (LaPrade type 4) (Figure 3B) associated to fracture of the external tibial plateau and deinsertion of the internal meniscus posterior root (LaPrade type 5) (Figure 3B) with meniscal extrusion (Figure 3C).
Results
Following the complementary tests, the patient was diagnosed with a complex meniscal and multiple ligament injury, and surgery was recommended. The latter was carried out after 7 days of admission, due to the need for medical optimization after the initial polytraumatism involving important chest and scapular contusion.
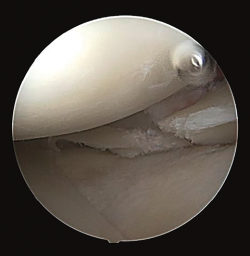
Arthroscopy confirmed the diagnosis by visualizing the avulsed root and bone fragment at medial level (Figure 4A) and the radial lesion of the external root (Figure 5). Palpation of both roots evidenced clear instability. The ACL was greatly affected, with subtotal rupture, while the PCL presented correct stability in response to palpation and testing.
The medial root avulsion fracture was repaired using a standard transtibial pullout technique(1,3,6). Suturing required the use of no. 2 FiberWire® (Arthrex, Naples, FL, USA ) through the root with the Knee Scorpion™ system (Arthrex, Naples, FL, USA) (Figure 4B). A FlipCutter® III retrograde reamer (Arthrex, Naples, FL, USA) with a Unicorn Meniscal Root (UMR) guide (Arthrex, Naples, FL, USA) was used to drill a blind tibial tunnel, 6 mm in diameter and 15 mm in length, from the bone bed of the medial meniscus towards the anteromedial tibial cortical layer. The meniscus sutures were retrieved through the trans-bone tunnel with a FiberStick® (Arthex, Naples, FL, USA). The suture was knotted through a metal button, securing correct reduction of the meniscal avulsion (Figure 4C).
The rupture of the lateral meniscal root was repaired with two U-shaped meniscal sutures using a Knee Scorpion™ suture passer. Lastly, reconstruction of the ACL was carried out with an anterior tibial tendon allograft with proximal and distal cortical suspension fixation according to the all-inside technique, avoiding the coalition of tunnels at tibial medial level.
With regard to postoperative rehabilitation, a postsurgery knee pad was used with varus/valgus control and without posterior drawer control, since the operated ACL injury was considered to be more relevant than the PCL lesion. The pad was removed 8 weeks after surgery. The avoidance of weight bearing of the affected leg was included during four weeks to avoid meniscus tension, followed by partial weight bearing for another four weeks. Flexion of the knee controlled with the orthosis was restricted to 30º during the first two weeks, followed by a gradual increase to 60º and 90º after two and four weeks, respectively, to protect the meniscal repairs in relation to both the medial avulsion and the lateral suture(8).
Four months after the operation, control MRI revealed correct positioning of both menisci, with no evidence of meniscus extrusion (Figure 6A), and with consolidation of the reinserted fragment (Figure 6B). The ACL plasty was seen to be intact and correctly positioned (Figure 6C). At physical examination, the joint balance of the knee comprised a 5º defect for complete extension, with a passive flexion range of 120º and an active range of 100º, with correct anteroposterior and mediolateral stability.
Discussion
The meniscal roots are the only part of the meniscus inserted in bone, and damage to them is likely to have a strong negative effect upon the biomechanics of the knee. As a result, in recent years, the main reference groups have placed emphasis on the importance of the diagnosis and treatment of these lesions(3,9).
Root tears are commonly soft tissue lesions involving either the ligament of the root or the posterior meniscal horn(2,10,11). Root avulsion fractures are rare lesions with few literature references(12). Although such avulsions can be evidenced by MRI, it is also advisable to obtain radiographs and conduct a CT study for improved visualization of the avulsed bone fragment, in addition to the routine resonance imaging study made when meniscus and ligament injuries are suspected. The characteristics of our patient (a young male with severe trauma) are consistent with those described in the literature(11). Surgeons should exercise a strong degree of suspicion in patients of this kind, particularly if the radiographic study evidences a bone fragment near the insertion of the meniscal root(12). High energy mechanisms may associate damage to the lateral or central pivot ligaments, particularly the ACL. At the time of rupture of this ligament, the lateral femoral condyle may subsequently suffer subluxation over the tibia, exerting great tension in the posterior horn of the lateral meniscus(4), causing the lesion. Tears of the posterior root of the lateral meniscus have been identified in up to 7-12% of all patients with ACL injuries(2,4,5); for this reason, it is important to always discard their presence in young patients with high energy knee injuries. In a study in cadavers, Markolf(13) showed anterior tibial force and external tibial torsion to be loading modes that generate great forces in the posterior medial root, presumably through trapping of the medial femoral condyle against the posterior horn of the medial meniscus. Elimination of the ACL even increases the force acting upon the posterior medial root(13). This study may explain the mechanism underlying the medial lesion observed in our patient.
There is broad agreement in the literature that root tear fixation is the treatment of choice for preserving the biomechanical function of the meniscus(1,10,14). Since root avulsion fractures probably exert the same harmful effect upon the biomechanics of the knee joint as root injuries without bone involvement, we believe that fixation always should be indicated if possible in both lesion patterns. Direct fixation systems have been described for avulsions, involving the placement of sutures through the bone fragment; alternatively, indirect fixation can be performed, positioning the sutures adjacent to the fragment (2,5,12,14). It is very advisable for these fixation systems to be routinely available for use in the different root injuries in arthroscopic ligament repair surgeries, for as commented above, it is not unusual to find this combination of lesions even unexpectedly(2,4,5). Indirect fixation was carried out in our patient, since the fragment was small, and we sought to avoid its fracture during the manoeuvre.
Since ACL insufficiency is associated to failed meniscal repair(14), reconstruction of the ACL is indicated in these cases(3,6,11), based on autologous or heterologous grafts - this being the system used in our case in order not to increase morbidity of the soft tissues around the knee.