Perioperative pain management in arthroscopic surgery of the shoulder
Manejo perioperatorio del dolor en cirugía artroscópica de hombro
Resumen:
El control perioperatorio del dolor es de gran importancia no solo para el confort inmediato del paciente, sino porque constituye un factor limitante del resultado final de la cirugía.
A pesar de existir una amplia variedad de alternativas terapéuticas, actualmente no está del todo claro cuál es la mejor opción para hacer frente al dolor en términos de eficacia y seguridad. Se realiza una revisión crítica de la literatura sobre los aspectos que permiten manejar de forma adecuada el dolor perioperatorio. Es útil realizar una medición adecuada del dolor con escalas específicas.
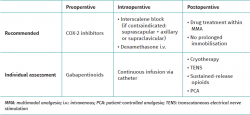
En el preoperatorio, se recomienda el uso de antiinflamatorios no esteroideos (AINE) inhibidores de la COX-2. Los gabapentinoides pueden ser útiles cuando se sospeche la aparición de náuseas o vómitos tras la intervención quirúrgica.
Intraoperatoriamente, el empleo de bloqueos interescalénicos con aplicación en bolo del anestésico local es la medida más recomendada. En caso de patología pulmonar severa, se pueden utilizar bloqueos del supraescapular con bloqueo del axilar asociado, salvo si durante el procedimiento se va a actuar principalmente sobre las estructuras anteriores del hombro, en cuyo caso se recomienda emplear bloqueos supraclaviculares. En cirugías particularmente dolorosas, se debe valorar el empleo de infusión continua de anestésico a través de un catéter interescalénico.
Durante el postoperatorio, se recomienda el uso de protocolos de analgesia multimodal (AMM). El uso de AINE postoperatorios se recomienda en artroscopias de inestabilidad glenohumeral y cuando no se realiza una reparación del manguito rotador. Si se lleva a cabo, se debe valorar individualmente su uso, ya que este podría estar relacionado con una peor cicatrización de la interfase tendón-hueso. La inmovilización prolongada aumenta los niveles de dolor en el postoperatorio inmediato. El empleo de crioterapia y electroestimulación nerviosa transcutánea (TENS) postoperatorios pueden ser de ayuda para reducir la sensibilidad nociceptiva. La administración de pautas cortas de opioides de liberación prolongada es una alternativa a los protocolos de AMM, así como la analgesia controlada por el paciente, en sus diferentes modalidades.
Abstract:
Perioperative pain control is very important not only for the immediate comfort of the patient but also because it constitutes a limiting factor for the final outcome of surgery.
Despite the existence of a broad range of management alternatives, the best strategy for dealing with pain in terms of efficacy and safety is not currently fully clear. A critical literature review is made of the aspects that can facilitate the adequate management of perioperative pain. It is useful to perform adequate pain assessment based on the use of specific scales.
In the preoperative phase, the use of COX-2 inhibiting nonsteroidal anti-inflammatory drugs (NSAIDs) is recommended. Gabapentinoids may be useful when the appearance of nausea or vomiting is suspected after surgery.
Intraoperatively, the use of interscalene block with local anaesthetic bolus dosing is the most widely recommended measure. In patients with serious lung disease, suprascapular block with associated axillary block may be used, except if surgery is mainly focused on the anterior structures of the shoulder — in which case supraclavicular block is advised. In particularly painful surgery, continuous anaesthetic infusion through an interscalene catheter should be considered.
In the postoperative phase, the use of multimodal analgesia (MMA) protocols is recommended. Postoperative NSAID use is advised in glenohumeral instability arthroscopy and when no rotator cuff repair is performed. If done, individual assessment of use is required, since it may be related to poorer healing of the tendon-bone interface. Prolonged immobilisation increases pain levels in the immediate postoperative period. Postoperative cryotherapy and transcutaneous electrical nerve stimulation (TENS) may be useful for reducing nociceptive sensitivity. Short sustained-release opioid regimens are an alternative to MMA protocols, in the same way as patient-controlled analgesia in its different modalities.
Introduction
Shoulder arthroscopy is one of the most common procedures in orthopaedic surgery. With the advances in both surgical and anaesthetic techniques, it is increasingly common for shoulder arthroscopy to be performed in ambulatory major surgery units, allowing early patient discharge, faster postoperative recovery and a decrease in costs related to hospital admission. However, the management of postoperative pain is a genuine challenge for the surgical team, not only because of its impact upon the patient but also because it is known to influence the final outcome of the process(1).
Different strategies have been described for dealing with pain in shoulder arthroscopy. The traditional approach has been to administer opioid analgesics via the oral or parenteral route. However, in reducing the pain to acceptable levels, complications may occur in the form of nausea, drowsiness or the development of drug dependence(2). Traditional management in turn has been followed by the development of different analgesic techniques such as regional anaesthesia, early physiotherapy protocols, the continuous infusion of local anaesthetic both intraarticular and within the subacromial space, continuous flow cryotherapy, or MMA regimens(3). Despite this broad range of management alternatives, the best strategy for dealing with pain in terms of efficacy and safety is not currently fully clear.
The present study offers a narrative review of the literature on the different options for treating perioperative pain in shoulder arthroscopy. The aim is to summarise the most relevant information and establish clear recommendations that can guide the arthroscopist when dealing with patients with shoulder disease conditions.
Importance of perioperative pain in arthroscopic surgery of the shoulder
Pain frequently develops following shoulder arthroscopy, with a strong impact upon the final outcome of the process. Up to 20% of all patients report maximum pain levels on the day after hospital discharge(4). The pain varies in intensity over the days, and may be lower on the day of surgery and on the following day compared with the days before the operation. Peak pain intensity is reached on days 2, 3 and 4 after surgery(5). From day 30 the sudden changes in pain intensity disappear, followed by stabilisation until the end of the process.
Not all surgical procedures are equally painful, and not all patients perceive pain in the same way. In this regard, higher pain levels have been described in rotator cuff repair procedures(5,6), which can be up to 2.6 times more painful than glenohumeral instability surgeries during the first 24 hours. From day two these differences tend to disappear, though rescue opioid use remains higher in rotator cuff repair procedures during the first postoperative week(6). The patient-dependent factors correlated to greater postoperative pain intensity are the female gender and a history of anxiety and/or depression(7). The presence of psychosocial problems before surgery, such as being unemployed, or emotional disorders, are also associated to greater levels of pain after the operation(8,9).
Studies have been made to determine whether perioperative pain may be a risk factor for the development of other complications and not constitute only an outcome variable. The risk factors for recurrent rotator cuff rupture following arthroscopic repair have been widely analysed, and it has not been possible to clearly establish whether perioperative pain is one of them(10). However, the appearance of intense pain during the immediate postoperative phase may predispose to shoulder stiffness three months after rotator cuff repair(11). Furthermore, an inverse relationship has been described between the degree of patient satisfaction after cuff repair and pain intensity before surgery and during the immediate postoperative period(12). Therefore, perioperative pain control is very important not only for the immediate comfort of the patient but also because it constitutes a limiting factor for the final outcome of surgery.
Assessment of pain in arthroscopic surgery of the shoulder
In order to treat postoperative pain, it must be quantified using adequate tools that are easily reproducible, with due therapeutic correlation, and that can be completed by the patients themselves.
Many validated scales are available for the assessment of shoulder joint function. Most of them include pain as an assessment item, but they are not designed to exclusively quantify pain.
Specific pain assessment scales are divided into unidimensional and multidimensional constructs. Unidimensional scales are commonly used in view of their simplicity, but they do not assess the complexity and multifactorial cause of the pain. This group includes the visual analogue scale (VAS) and the numerical scale. Multidimensional scales in turn afford a more complete evaluation of the characteristics of pain — the most widely used construct being the Brief Pain Inventory, which was originally developed for application to cancer pain, though it is widely used in clinical practice and research to evaluate the intensity and impact of pain, and the effect of analgesic treatment. There are two versions (long and brief), and both have been validated in Spanish(13).
Preoperative management
Preventive analgesia, understood as medication use before surgery with the aim of reducing postoperative pain, has often been used in arthroplasty surgery of the knee and hip, with good outcomes in terms of effectiveness and safety(14). However, there is little evidence on its use in shoulder arthroscopy.
Nonsteroidal anti-inflammatory drugs
Both non-selective and selective (COX-2 inhibiting) nonsteroidal anti-inflammatory drugs (NSAIDs) have been used as preventive analgesia in shoulder arthroscopy, with a preference for the COX-2 inhibitors, due to their better gastrointestinal profile ((15). Toivonen et al. carried out a placebo-compared clinical trial of 30 patients administered with 120 mg of etoricoxib one hour before arthroscopic subacromial decompression(16). They found pain in the first hours after surgery to be less intense in the treatment group, and the benefit was moreover maintained for up to 7 days after the operation. Likewise, there was a significantly lesser need for rescue analgesia than in the placebo group. In a comparative series versus placebo, Rohuani et al. found that the administration of 200 mg of celecoxib every 12 hours two days before arthroscopic rotator cuff repair significantly reduced the pain up to 48 hours after surgery, with a lesser need for rescue opioids, and improved patient nocturnal rest(15). Likewise, the percentage of patients who suffered nausea or vomiting decreased 43% on administering celecoxib.
On the other hand, the use of NSAIDs is not without adverse events. Apart from the gastrointestinal and cardiovascular problems associated with their use in general (particularly the non-selective drugs), NSAIDs may also interfere with the healing process at the tendon-bone interface, which for example would affect the recurrent rupture rates of rotator cuff repair surgery. However, the data found in the literature are referred only to animal models on one hand, and to the postoperative use of NSAIDs on the other; it therefore cannot be affirmed whether such complications may appear when these drugs are administered preoperatively.
Gabapentinoids
Gabapentinoids (gabapentin and pregabalin) administration has been widely investigated in the preoperative setting due to their analgesic and, to a lesser extent, anxiolytic effects(17,18,19,20). Gabapentin has been used at variable doses between 300-800 mg administered two hours before shoulder arthroscopy in different placebo-compared clinical trials, with variable results in terms of pain reduction(19,20). J. Galindo-Avalos et al., in a meta-analysis of clinical trials, found gabapentinoids to reduce pain 24 hours after shoulder arthroscopy. The reduction was statistically significant but scantly relevant from the clinical perspective (0.77 points on the VAS) — though there was a more marked decrease in the need for rescue opioids(18). The most interesting effect of the preoperative administration of gabapentinoids was a 10% decrease in the probability of nausea or vomiting in the first 24 hours after surgery. These drugs therefore could represent a valid alternative in cases where it is suspected that such complications may occur(17).
Opioids
There is little literature support of the preoperative administration of opioids in shoulder arthroscopy. As an anecdote, application within the subacromial space of 20 mg of morphine in 10 ml of saline solution 20 minutes before arthroscopic rotator cuff repair has been shown to be effective in reducing pain versus placebo, and the effect was maintained for up to two weeks after surgery, with no reported complications(21). However, no reference has been found regarding oral, transdermal or intravenous administration before surgery.
Considering the above, the preoperative use of COX-2 inhibiting NSAIDs in shoulder arthroscopies is recommended. Gabapentinoids are advised when nausea or vomiting is suspected to occur in the first hours after surgery.
Intraoperative management
During the intraoperative period, brachial plexus nerve block is currently considered to be the reference technique for controlling pain in shoulder arthroscopy(22). There is abundant scientific evidence on the effectiveness of such block procedures compared with the isolated administration of oral or intravenous analgesics(23). In addition, their safety has been widely evidenced and has been consolidated thanks to the development of ultrasound-guided techniques that allow direct visual control of the region to be anaesthetised(24). Most of the described adverse effects are infrequent and usually resolved spontaneously(25).
Interscalene blocks
A number of nerve blocks are available, depending on the targeted region of the brachial plexus. The most popular options are the interscalene blocks, in which the anaesthetic is applied around roots C5 and C6, which posteriorly conform the superior and middle trunks of the brachial plexus from which the nerve roots responsible for nociceptive sensitivity of the cutaneous region of the entire shoulder, glenohumeral joint and subacromial space arise. The popularity of these procedures is attributable to their acknowledged efficacy. Following rotator cuff repair, the maximum pain score according to the VAS is up to 50% lower in the first 24 hours when interscalene block is performed versus parenteral opiate dosing. In addition, 33-70% of all patients require no additional analgesia during hospital admission(23,26). The analgesic benefit persists for up to 24 hours longer than with the isolated administration of opioids(27,28), while the scores on the Constant scale remain better until the sixth postoperative week after rotator cuff repair(23). This was reported by Gurger et al. in a randomised clinical trial of 85 patients in which interscalene blocks were compared against isolated general anaesthesia for arthroscopic rotator cuff repair. The authors explained their findings in terms of the lesser pain experienced by the patients in the immediate postoperative period, which encouraged them to be more active — thus improving function even though the effect of the block had disappeared(23). Logically, the movements and gestures which patients can make following rotator cuff repair are dependent upon the postoperative rehabilitation protocol determined by the surgeon, though the fact that the patients do not suffer pain encourages them to perform the allowed exercises.
Warrender et al. conducted a systematic review of clinical trials on treatments for pain following shoulder arthroscopy in ambulatory surgery units. In addition to confirming good outcomes in terms of pain in the first hours after surgery, they found nausea and vomiting to decrease 13% in the immediate postoperative period versus placebo(27). As a result of these favourable data, the authors recorded shorter patient stays in the ambulatory surgery units(27). A more recent systematic review and meta-analysis of clinical trials referred to this same topic was published by Hurley et al. These authors confirmed the good outcomes described above, to the point of using the results of interscalene blocks as a reference for comparing the rest of the brachial plexus block procedures(28).
Interscalene block procedures are not without adverse effects, however. Homolateral diaphragmatic paralysis may occur in up to 78.7% of all cases(25). Although such paralysis is usually partial and is well tolerated by individuals who have a good lung reserve, the consequences may be very negative for patients with previous pulmonary disease conditions, this representing a relative contraindication to the use of such techniques. Horner's syndrome may appear in 10-28.2% of the patients(22), and paresis maintained beyond the first 24 hours may be observed in 14.2% of the cases(22). Nevertheless, all these complications tend to be self-limiting in time, and only rarely interfere with global patient satisfaction. This circumstance, together with the fact that serious complications such as vascular damage, pneumothorax due to puncture or sustained nerve damage are practically anecdotal situations(29), allows us to affirm that interscalene blocks are safe techniques. For all these reasons, the literature proposes interscalene block as the reference technique for controlling pain in shoulder arthroscopy(27,28).
Supraclavicular blocks
Supraclavicular block procedures appear as an alternative to interscalene blocks seeking to avoid the complications associated to the latter, particularly diaphragmatic paralysis in patients with existing lung disease. Under ultrasound guidance, we can locate the anterior and posterior division of the superior trunk of the brachial plexus within the supraclavicular fossa. The application of anaesthetic at this level has yielded good results in absolute terms referred to pain reduction. Schubert et al. conducted a systematic review with meta-analysis of clinical trials comparing the results of supraclavicular block procedures versus interscalene blocks in treating postoperative pain after shoulder surgery (not only arthroscopic procedures)(30). With the supraclavicular techniques, the authors found the mean VAS score in the anaesthesia recovery units to be 1.1 points versus 2.1 points 24 hours after surgery. Guo et al., in another meta-analysis of clinical trials comparing supraclavicular blocks versus interscalene block procedures in shoulder surgery (not only arthroscopic procedures), found that only 3.2% of the patients subjected to supraclavicular block required opiate rescue analgesia during hospital admission(31).
In relation to interscalene blocks, Schubert et al. found that while pain reported in the post-anaesthesia recovery unit was significantly lower with interscalene block procedures, the difference was no longer significant in the first 24 hours(30). Likewise, there were no significant differences in the need for additional opioid use. On the other hand, Hurley et al. observed no significant differences in pain intensity assessed by the VAS or in the need for rescue analgesia between the interscalene and supraclavicular block procedures at any time during the first 24 hours after surgery(28). In contrast, in the study published by Schubert et al., adverse effects such as ipsilateral diaphragmatic paralysis, Horner's syndrome and hoarseness were seen to be more frequent in the case of interscalene blocks(30).
Suprascapular blocks
The suprascapular nerve is responsible for the sensory innervation of an extensive area of the posterior part of the glenohumeral capsule and the subacromial space. A number of studies have demonstrated the efficacy of selective suprascapular blocks compared with isolated general anaesthesia in arthroscopic rotator cuff repair, reducing the need for additional anaesthesia by up to 51% and opioid use after hospital discharge by 31%, and reducing the appearance of adverse effects such as nausea and vomiting up to 5-fold(32).
Compared with interscalene block, the effectiveness of suprascapular block is slightly lower, though with a lesser probability of complications. Different prospective studies have compared the two techniques. Kay et al. conducted a systematic review and meta-analysis of randomised clinical trials comparing suprascapular blocks versus interscalene blocks in shoulder arthroscopy procedures(22). A total of 14 studies were analysed, with the inclusion of 1382 patients. The authors found that, in the post-anaesthesia recovery units, the patients that had undergone interscalene blocks reported significantly less pain. In the course of the first 24 hours these differences lost statistical significance, though the tendency was clearly favourable to the group undergoing interscalene blocks. Beyond the first 24 hours, the pain scores were similar with both techniques. Likewise, 39-53% of the patients in the suprascapular block group required additional opioids in the post-anaesthesia recovery unit, versus only 12% of those in the interscalene block group. In the course of the following hours, these needs proved similar in both groups. These differences can be explained because suprascapular block does not achieve complete anaesthesia of all the shoulder region; some authors therefore propose combining it with selective axillary nerve block in order to increase the anaesthesia zone(33). Even so, the pain sensitivity of certain structures of the anterior shoulder region, particularly the anterior capsule and the subscapular area, are not fully covered by suprascapular and axillary block, this representing a relative limitation for the use of the technique. On the other hand, the incidence of complications was lower in the case of suprascapular block — particularly motor block sustained for over 24 hours, which occurred in 14.6% of the cases of interscalene block versus in only 1.5% of the suprascapular block procedures(22). It therefore can be concluded that although effective, suprascapular blocks are not more effective than interscalene blocks; consequently, the former should be used as an alternative when interscalene block is not indicated, as in patients with a serious lung disease.
Continuous infusion in nerve blocks
Extensive experience has been gained with continuous local anaesthetic infusion in the brachial plexus in different shoulder surgeries, both open and arthroscopic(34). Using a catheter, the anaesthetic is administered on a continuous basis, and there have even been descriptions of ambulatory physiotherapy protocols keeping the catheter in place during the first days after the operation(35).
In comparison with the administration of a single anaesthetic bolus dose, continuous infusion through a catheter affords better levels of analgesia at 24 hours, less sleep disturbance, and a lesser need for additional opioids during the first week after rotator cuff repair(36). Furthermore, it avoids the "rebound effect" characterised by a new rise in pain once the effect of analgesia administered as a bolus dose wears off. This was evidenced by Kim et al., who randomised patients subjected to arthroscopic rotator cuff repair to preoperative interscalene block as a bolus dose, interscalene catheter placement with continuous analgesia infusion, or analgesia with opioids upon demand(36). Fredrickson et al. carried out a clinical trial comparing local anaesthesia as a bolus dose in interscalene block versus catheter placement with continuous analgesia infusion for the treatment of pain following shoulder arthroscopy(37). The maximum pain levels were seen to be lower in the continuous infusion group on the first postoperative day, particularly during movements on the part of the patient. The pain levels equalised by day two after surgery. The use of rescue analgesia remained lower in the continuous infusion group during the first two days.
However, the need to retain the catheter for several days implies an increased incidence of adverse events (5-9%) — the most frequent being accidental catheter mobilisation, recorded in 3.6% of the patients(38). As an added inconvenience, in the absence of health infrastructure allowing home manipulation and removal of the catheter, hospital stay must be maintained for a longer period, and this in turn increases the costs(36). For these reasons, some authors consider that although continuous analgesia infusion systems are more effective than bolus dosing, their use is not justified in scantly or moderately painful surgeries(38). It is therefore necessary to individualise each case, taking different factors into account, such as the surgical procedure to be carried out, in order to choose the therapeutic option best suited to the patient.
Local anaesthetic infiltration
Intraarticular or subacromial single bolus dosing of local anaesthetic, as well as infiltration of the arthroscopy portals, has been a common practice in our setting. Scoggin et al., in a prospective placebo-controlled study, found bupivacaine administration in portals and at subacromial or intraarticular level to be effective in reducing pain during the first 60 minutes after surgery, though the pain levels subsequently equalised, with no decrease in the need for rescue opioids(39). Debnath et al. in turn found the analgesic effect to be 5 times more lasting when performing interscalene block than with isolated intraarticular or subacromial anaesthetic infiltration. Therefore, such isolated use is not recommended.
Based on the above, it is advisable to perform interscalene block procedures with bolus application of the local anaesthetic in order to treat pain in shoulder arthroscopies. In patients with serious lung disease, it is advisable to perform suprascapular block with associated axillary block, except if surgery is mainly focused on the anterior structures of the shoulder (anterior capsule, subscapular zone, etc.), in which case supraclavicular block is recommended. In particularly painful surgery, continuous anaesthetic infusion through an interscalene catheter may be considered.
Postoperative management
Cryotherapy
Cold application lowers local metabolism, reducing inflammation and pain. In shoulder surgery (not exclusively arthroscopic), cryotherapy has been associated to a significant decrease in opiate use and lesser pain sensation in the first hours after the operation, facilitating sleep on the following night and more active patient participation in the rehabilitation process(40). Furthermore, the effect of cold application does not appear to be limited to the first postoperative hours, since patients subjected to cryotherapy report lesser pain perception up to day 10 after surgery, despite the suspension of local cold application much earlier. The combination of cryotherapy with intermittent dynamic compression —widely used in knee surgery— has not been shown to offer greater benefit than the isolated application of local cold, probably because of the difficulty of developing devices that adapt to this anatomical region(41,42).
Immobilisation
Postoperative immobilisation influences the experienced pain levels. Patients subjected to longer periods of immobilisation present higher pain ranges throughout the recovery process(43). On comparing accelerated rehabilitation protocols with other more conservative strategies after rotator cuff repair surgery, the immobilisation and stiffness associated to the slow protocols result in higher pain levels in the early stage of rehabilitation. However, long-term (> 6 months) satisfaction proves similar(44), with poorer performance on the American Shoulder and Elbow Surgeons (ASES) scale in those repairs involving a rapid program — this possibly being related to a greater incidence of recurrent rupture in large injuries(45). Mazzocca et al. compared two rotator cuff rehabilitation models in single-tendon injuries: a slow protocol (28 days to the start of assisted mobility) versus an accelerated protocol (2 days). No differences in pain perception were noted during the entire follow-up. The functional scales in intermediate phases showed better scores in the accelerated rehabilitation group, though the scores equalised 6 months after surgery(46). The position of the arm during immobilisation does not appear to have much of an impact upon patient-reported pain. Hollman et al. compared immobilisation with a standard antirotatory sling versus a 30° abduction sling during the postoperative period of rotator cuff repair surgery, and recorded no differences in either pain intensity or analgesic use between the two groups(47).
Transcutaneous electrical nerve stimulation (TENS)
The efficacy of TENS in controlling pain in the postoperative period of shoulder surgery was evaluated by Mahure et al. in a placebo-controlled study involving cuff suturing. The authors recorded a decrease in pain at 48 hours and 7 days after the operation, with a lesser need for analgesics, in favour of the TENS group(48). In the mentioned study, TENS was applied personally by the patient from the immediate postoperative period to day 7 after surgery, in the form of four daily sessions, each with a duration of 45 minutes.
Postoperative pharmacological therapy within multimodal analgesia
Multimodal analgesia (MMA) refers to the use of various therapeutic alternatives aimed at securing adequate pain control. This includes the combination of preoperative analgesia, nerve blocks, local infiltrations, postoperative analgesia, etc., used in sequence and in a protocolised manner to achieve an adequate analgesic effect with the fewest complications possible. Postoperative pharmacological therapy is a very important element in this regard. The pondered use of different analgesic agents with synergic actions makes it possible to reduce their individual doses and therefore the risk of side effects, while maximising their benefits.
The analgesics commonly used in MMA are NSAIDs — both non-selective and selective (COX-2 inhibitors) — α2 agonists, glucocorticoids, antagonists of the glutamine receptors or NMDA (N-methyl-d-aspartate), antiepileptics (gabapentin, pregabalin), antidepressants and opioids. This blocks the pain generators at different points of the nociceptive pathways, which has been shown to exert a synergic effect affording more potent analgesia than blocking of the pain pathways at a single isolated point(49). The end result is greater patient satisfaction, lesser opioid use, fewer complications and a reduction of medical costs.
In relation to shoulder arthroscopic surgery, MMA has also been seen to exert favourable effects. Elkassabany et al. evaluated an MMA protocol (preoperative paracetamol and gabapentin, intraoperative NSAIDs and postoperative paracetamol, NSAIDs and gabapentin, with rescue oxycodone) versus opioids upon demand, in patients subjected to shoulder arthroscopy in the ambulatory major surgery setting. The authors recorded improved pain control during both activity and sleep, lesser opioid use, and greater satisfaction among the patients administered with MMA, both in the immediate postoperative period (24-48 hours) and at 7 days after surgery(4). The postoperative NSAIDs were maintained for a maximum of 72 hours.
As has been commented above, NSAID use is not without adverse effects, particularly in relation to healing of the repaired tendon-bone interface. Studies in animals models have shown that the use of both non-selective NSAIDs and COX-2 inhibitors complicates tendon healing in the animal rotator cuff, due to an alteration of collagen fibre distribution, which results in generalised weakness of the mentioned interface(50,51).
In relation to the clinical studies, Oh et al. carried out a clinical trial comparing celecoxib, ibuprofen and tramadol administration during the first 14 days after arthroscopic rotator cuff repair(52). At 24 months after surgery, the recurrent rupture rate was 37% in the celecoxib group, 7% in the ibuprofen group and 4% in the tramadol group (p = 0.009). Blomquist et al. in turn conducted a retrospective comparative study of patients administered with NSAIDs versus patients not given such medication in the first 7 days following arthroscopic Bankart repair. No statistically significant differences were observed in terms of the clinical outcomes or instability relapse rate(53). In a more general manner, Constantinescu et al. carried out a systematic review to analyse the influence of perioperative NSAID administration upon soft tissue healing in different sports trauma surgeries. The authors concluded that there is not enough evidence to indicate that any NSAID may have a deleterious effect upon healing of the tendon-bone interface(54).
In 2019, the PROSPECT (Procedure Specific Postoperative Pain Management) group performed a systematic review on the treatment of postoperative pain in rotator cuff surgery, with the aim of establishing a management guide. In their conclusions, the group recommended the use of NSAIDs and paracetamol before, during and after surgery, without specifying the duration of the treatment; the use of interscalene block of the brachial plexus as first choice and, as an alternative, suprascapular block with or without axillary block; an isolated pre- or intraoperative dose of intravenous dexamethasone to prolong the plexus action time, reducing the use of analgesics and antiemetic agents in the immediate postoperative period; and the reservation of opioids as rescue analgesia during the postoperative stage(55).
A valid alternative to the MMA protocols is the administration of short cycles of sustained-release opioids. Garnaud et al., in a nonrandomised prospective study, evaluated four models of analgesic treatment in ambulatory arthroscopic shoulder surgery. Group 1 received 100 mg of tramadol every 4 or 6 hours as postoperative treatment. Group 2 received 120 mg every 24 hours of nefopam in elastomer with continuous infusion and tramadol 100 mg as rescue measure. Group 3 received 10 mg of oxycodone every 4 or 6 hours. Group 4 received 20 mg of sustained-release oxycodone during 48 hours with 10 mg of oxycodone as rescue measure. All the groups were operated upon under general anaesthesia and interscalene plexus block, with the intraoperative administration of paracetamol, NSAIDs, dexamethasone and nefopam. The study treatments were started at discharge and lasted two days. At 5 days, superior pain control and patient satisfaction were recorded with sustained-release opioids. The authors concluded that sustained-release opioid administration in a short cycle of 48 hours afforded better pain control than tramadol or analgesia upon demand, with a reduction of the risk of complications and addiction problems(56). However, they indicated that sustained-release opioid administration in a short cycle did not exclude the need to manage the most common complications such as nausea and constipation, and that due attention should be focused on the patient risk factors for opioid abuse and dependence.
Continuous subacromial / intraarticular infusion
Continuous anaesthetic dosing through a catheter placed in the glenohumeral joint or subacromial space has been proposed as an alternative for the management of pain following shoulder arthroscopy procedures.
An et al. conducted a systematic review with meta-analysis of clinical trials comparing the results of continuous subacromial infusion versus placebo in shoulder arthroscopy focused on this anatomical space. The authors documented no benefit in terms of pain reduction during the first 48 hours, and rescue opioid use was only reduced at 12 hours after surgery(57). In relation to interscalene blocks, different prospective comparative studies have found both patient-reported pain intensity and rescue analgesia use to be lower with interscalene blocks — the differences being maintained up to day 6 after surgery(58,59). On the other hand, the adverse events rate associated to subacromial infusion is very low, and is more dependent upon the type of drug used(27).
There is currently little scientific evidence on the continuous intraarticular infusion of local anaesthetic. Scoggin et al. recorded analgesic benefit in the first 60 minutes after shoulder arthroscopy versus placebo in their randomised prospective study, but the authors did not assess the results for longer periods of time after the operation(39). The main complication of the intraarticular infusion of local analgesic is glenohumeral chondrolysis, which is recorded in up to 63% of all cases in which it was used, according to the retrospective case series published by Hansen et al.(60). Due to this high incidence and the great seriousness of the disorder, different reviews on this topic currently do not recommend a continuous infusion of local anaesthetic within the glenohumeral space(27,61).
Patient-controlled analgesia (PCA)
Patient-controlled analgesia (PCA) is a modality of postoperative pain control in which the patient personally decides when and how much analgesia is needed, according to the level of pain experienced. Administration can be made via different routes. In shoulder arthroscopy, the most widely studied options are the intravenous route and subacromial infusion through a catheter. Such analgesia requires important collaboration from the patient, who preoperatively receives instructions on the utilisation of the analgesia device and the limits of the technique.
Cho et al. carried out a randomised clinical trial comparing the outcomes of PCA via the intravenous route versus a subacromial catheter after shoulder arthroscopy and up to 72 hours after the operation. No differences were observed between the two techniques(62). Kim et al. in turn carried out another randomised clinical trial comparing interscalene block involving a bolus dose of local anaesthetic versus PCA through an interscalene catheter for treating pain after arthroscopic rotator cuff repair procedures. In the first two hours after the operation, the patients reported less pain with interscalene block; however, from 12 hours after surgery, with onset of the "rebound effect", the results were inverted, and the patients with PCA experienced comparatively less pain(36). Beyond the first 48 hours, the differences between the two groups disappeared.
Based on the above, it is advisable to use MMA protocols as the most important measure for controlling pain in shoulder arthroscopy. Within these protocols, COX-2 inhibiting NSAIDs are advised in glenohumeral instability arthroscopy and when no rotator cuff repair is performed. If done, individual assessment of use is advised, since such treatment may be related to poorer healing of the tendon-bone interface. Prolonged immobilisation increases pain levels in the immediate postoperative period. Postoperative cryotherapy and TENS may be useful for reducing nociceptive sensitivity. Short sustained-release opioid regimens are an alternative to MMA protocols, in the same way as PCA in its different modalities.
A number of recommendations are made in Table 1 as a summary of the most important issues addressed in this study for reducing perioperative pain in shoulder arthroscopy.
Conclusions
- The preoperative administration of COX-2 inhibitors is effective in reducing pain after shoulder arthroscopy.
- Preoperative gabapentinoids reduce the incidence of nausea and vomiting after the operation.
- Interscalene nerve block is the most effective analgesic measure, and thus should be regarded as the reference technique against which the rest of therapeutic options are compared.
- Suprascapular nerve blocks associated to axillary nerve block and supraclavicular block are the alternative to interscalene blocks when the latter is not indicated, as in patients with serious lung disease.
- Intravenous dexamethasone administration increases the effect and duration of nerve block.
- Multimodal analgesia protocols are able to reduce pain levels in the immediate postoperative period and in the days following the operation, using a reduced dose of different drugs.
- Prolonged immobilisation with a sling implies greater pain levels during the entire recovery period, particularly during the early stages of patient rehabilitation.
- Individualised evaluation of the characteristics of each patient and of each surgical procedure is required in order to choose the most effective analgesic techniques in each case.
Información del artículo
Cita bibliográfica
Autores
Pablo Carnero Martín de Soto
Arthrosport Zaragoza
Instituto Malagueño de Traumatología del Deporte (IMATDE). Málaga
Hospital Regional de Málaga
Abel Gómez Cáceres
Instituto Malagueño de Traumatología Deportiva (IMATDE). Málaga
Ignacio de Rus Aznar
Servicio de Cirugía Ortopédica y Traumatología. Clinica CEMTRO. Madrid
Unidad de Hombro y Codo. Hospital Universitario Ramón y Cajal. Madrid
Servicio de Cirugía Ortopédica y Traumatología. Hospital Monográfico Asepeyo Coslada. Madrid
Hospital Universitario de Torrejón. Madrid
Mikel Martiarena Moreno
Unidad de Hombro y Codo. Hospital Universitario Ramón y Cajal. Madrid
Jorge Díaz Heredia
Cirugía Ortopédica y Traumatología. Unidad de Hombro y Codo. Hospital Universitario Ramón y Cajal. Madrid
Clínica La Antigua. Guadalajara
Editor asociado de REACA
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Bishop JY, Sprague M, Gelber J, et al. Interscalene regional anesthesia for arthroscopic shoulder surgery: a safe and effective technique. J Shoulder Elbow Surg. 2006;15(5):567-70.
-
2D’Alessio JG, Rosenblum M, Shea KP, Freitas DG. A retrospective comparison of interscalene block and general anesthesia for ambulatory surgery shoulder arthroscopy. Reg Anesth. 1995;20(1):62-8.
-
3Uquillas CA, Capogna BM, Rossy WH, Mahure SA, Rokito AS. Postoperative pain control after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016;25(7):1204-13.
-
4Elkassabany NM, Wang A, Ochroch J, Mattera M, Liu J, Kuntz A. Improved Quality of Recovery from Ambulatory Shoulder Surgery After Implementation of a Multimodal Perioperative Pain Management Protocol. Pain Med. 2019;20(5):1012-9.
-
5Stiglitz Y, Gosselin O, Sedaghatian J, Sirveaux F, Molé D. Pain after shoulder arthroscopy: a prospective study on 231 cases. Orthop Traumatol Surg Res. 2011;97(3):260-6.
-
6Calvo E, Torres MD, Morcillo D, Leal V. Rotator cuff repair is more painful than other arthroscopic shoulder procedures. Arch Orthop Trauma Surg. 2019;139(5):669-74.
-
7De Boer FA, Schouten TTJ, Boekestein EP, et al. Risk factors for postoperative pain in the first three weeks after arthroscopic or open shoulder surgery. Orthop Traumatol Surg Res. 2019;105(2):241-4.
-
8Strube P, Schöpe T, Hölzl A, Brodt S, Matziolis G, Zippelius TK. Influence of Anxiety and Depression, Self-Rated Return-to-Work Problems, and Unemployment on the Outcome of Outpatient Rehabilitation After Shoulder Arthroscopy. Am J Phys Med Rehabil. 2019;98(12):1118-24.
-
9Panattoni N, Longo UG, De Salvatore S, et al. The influence of psychosocial factors on patient-reported outcome measures in rotator cuff tears pre- and post-surgery: a systematic review. Qual Life Res. 2022 Jan;31(1):91-116.
-
10Zhao J, Luo M, Pan J, et al. Risk Factors Affecting Rotator Cuff Retear After Arthroscopic Repair: a meta-analysis and systematic review. J Shoulder Elbow Surg. 2021 Nov;30(11):2660-70.
-
11Guity MR, Sobhani Eraghi A, Hosseini-Baharanchi FS. Early postoperative pain as a risk factor of shoulder stiffness after arthroscopic rotator cuff repair. J Orthop Traumatol. 2021;22(1):25.
-
12Tonotsuka H, Sugaya H, Takahashi N, Kawai N, Sugiyama H, Marumo K. Preoperative Pain Control in Arthroscopic Rotator Cuff Repair: Does It Matter? Clin Orthop Surg. 2019;11(2):192-9.
-
13De Andrés Ares J, Cruces Prado LM, Canos Verdecho MA, et al. Validation of the Short Form of the Brief Pain Inventory (BPI-SF) in Spanish Patients with Non-Cancer-Related Pain. Pain Pract. 2015;15(7):643-53.
-
14Díaz-Heredia J, Loza E, Cebreiro I, Ruiz Ibán MÁ. Preventive analgesia in hip or knee arthroplasty: a systematic review. Rev Esp Cir Ortop Traumatol. 2015;59(2):73-90.
-
15Rouhani A, Tabrizi A, Elmi A, Abedini N, Mirza Tolouei F. Effects of preoperative non-steroidal anti-inflammatory drugs on pain mitigation and patients’ shoulder performance following rotator cuff repair. Adv Pharm Bull. 2014;4(4):363-7.
-
16Toivonen J, Pitko V, Rosenberg PH. Etoricoxib pre-medication combined with intra-operative subacromial block for pain after arthroscopic acromioplasty. Acta Anaesthesiol Scand. 2007;51(3):316-21.
-
17Bang SR, Yu SK, Kim TH. Can gabapentin help reduce postoperative pain in arthroscopic rotator cuff repair? A prospective, randomized, double-blind study. Arthroscopy. 2010;26(9 Suppl):S106-11.
-
18Galindo-Ávalos J, Colin-Vázquez A, López-Valencia J, Gómez-Gómez JM, Bernal-Fortich LD. Eficacia y seguridad de la analgesia preventiva con gabapentinoides para pacientes sometidos a cirugía artroscópica de hombro: una revisión sistemática y metaanálisis. Acta Ortop Mex. 2019;33(6):416-23.
-
19Adam F, Ménigaux C, Sessler DI, Chauvin M. A single preoperative dose of gabapentin (800 milligrams) does not augment postoperative analgesia in patients given interscalene brachial plexus blocks for arthroscopic shoulder surgery. Anesth Analg. 2006;103(5):1278-82.
-
20Mardani-Kivi M, Karimi Mobarakeh M, Keyhani S, Haghighi M, Hashemi-Motlagh K, Saheb-Ekhtiari K. Arthroscopic Bankart surgery: Does gabapentin reduce postoperative pain and opioid consumption? A triple-blinded randomized clinical trial. Orthop Traumatol Surg Res. 2016;102(5):549-53.
-
21Khashan M, Dolkart O, Amar E, et al. Effect of preemptive intra-articular morphine and ketamine on pain after arthroscopic rotator cuff repair: a prospective, double-blind, randomized controlled study. Arch Orthop Trauma Surg. 2016;136(2):233-9.
-
22Kay J, Memon M, Hu T, et al. Suprascapular Nerve Blockade for Postoperative Pain Control After Arthroscopic Shoulder Surgery: A Systematic Review and Meta-analysis. Orthop J Sports Med. 2018;6(12):2325967118815859.
-
23Gurger M, Ozer AB. A comparison of continuous interscalene block versus general anesthesia alone on the functional outcomes of the patients undergoing arthroscopic rotator cuff repair. Eur J Orthop Surg Traumatol. 2019;29(8):1659-66.
-
24Bambaren IA, Domínguez F, Elías Martín ME, Domínguez S. Anesthesia and Analgesia in the Patient with an Unstable Shoulder. Open Orthop J. 2017;11:848-60.
-
25Holbrook HS, Parker BR. Peripheral Nerve Injury Following Interscalene Blocks: A Systematic Review to Guide Orthopedic Surgeons. Orthopedics. 2018;41(5):e598-e606.
-
26Krone SC, Chan VW, Regan J, et al. Analgesic effects of low-dose ropivacaine for interscalene brachial plexus block for outpatient shoulder surgery-a dose-finding study. Reg Anesth Pain Med. 2001;26(5):439-43.
-
27Warrender WJ, Syed UAM, Hammoud S, et al. Pain Management After Outpatient Shoulder Arthroscopy: A Systematic Review of Randomized Controlled Trials. Am J Sports Med. 2017;45(7):1676-86.
-
28Hurley ET, Maye AB, Thompson K, et al. Pain Control After Shoulder Arthroscopy: A Systematic Review of Randomized Controlled Trials With a Network Meta-analysis. Am J Sports Med. 2021;49(8):2262-71.
-
29Yan S, Zhao Y, Zhang H. Efficacy and safety of interscalene block combined with general anesthesia for arthroscopic shoulder surgery: A meta-analysis. J Clin Anesth. 2018;47:74-9.
-
30Schubert AK, Dinges HC, Wulf H, Wiesmann T. Interscalene versus supraclavicular plexus block for the prevention of postoperative pain after shoulder surgery: a systematic review and meta-analysis. Eur J Anaesthesiol. 2019;36(6):427-35.
-
31Guo CW, Ma JX, Ma XL, et al. Supraclavicular block versus interscalene brachial plexus block for shoulder surgery: a meta-analysis of clinical control trials. Int J Surg. 2017;45:85-91.
-
32Lee JJ, Yoo YS, Hwang JT, et al. Efficacy of direct arthroscopy-guided suprascapular nerve block after arthroscopic rotator cuff repair: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc. 2015;23(2):562-6.
-
33Checcucci G, Allegra A, Bigazzi P, Gianesello L, Ceruso M, Gritti G. A new technique for regional anesthesia for arthroscopic shoulder surgery based on a suprascapular nerve block and an axillary nerve block: an evaluation of the first results. Arthroscopy. 2008;24(6):689-96.
-
34Cohen NP, Levine WN, Marra G, et al. Indwelling interscalene catheter anesthesia in the surgical management of stiff shoulder: a report of 100 consecutive cases. J Shoulder Elbow Surg. 2000;9(4):268-74.
-
35Carnero-Martín de Soto P, Zurita-Uroz N, Calvo-Díaz Á. Resultados de la artrólisis artroscópica seguida de un programa de rehabilitación precoz ambulatoria con catéter interescalénico permanente como tratamiento de la rigidez secundaria de hombro. Rev Artrosc. 2020;27(02):41-6.
-
36Kim JH, Koh HJ, Kim DK, et al. Interscalene brachial plexus bolus block versus patient-controlled interscalene indwelling catheter analgesia for the first 48 hours after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2018;27(7):1243-50.
-
37Fredrickson MJ, Fredrickson MJ, Ball CM, Dalgleish AJ. Analgesic effectiveness of a continuous versus single-injection interscalene block for minor arthroscopic shoulder surgery. Reg Anesth Pain Med. 2010;35(1):28-33.
-
38Marhofer P, Anderl W, Heuberer P, et al. A retrospective analysis of 509 consecutive interscalene catheter insertions for ambulatory surgery. Anaesthesia. 2015;70(1):41-6.
-
39Scoggin JF, Mayfield G, Awaya DJ, Pi M, Prentiss J, Takahashi J. Subacromial and intra-articular morphine versus bupivacaine after shoulder arthroscopy. Arthroscopy. 2002;18(5):464-8.
-
40Speer KP, Warren RF, Horowitz L. The efficacy of cryotherapy in the postoperative shoulder. J Shoulder Elbow Surg. 1996;5(1):62-8.
-
41Kraeutler MJ, Aberle NS, Brown CC, Ptasinski JJ, McCarty EC. Clinical Outcomes and Return to Sport After Arthroscopic Anterior, Posterior, and Combined Shoulder Stabilization. Orthop J Sports Med. 2018;6(4):2325967118763754.
-
42Alfuth M, Strietzel M, Vogler T, Rosenbaum D, Liem D. Cold versus cold compression therapy after shoulder arthroscopy: a prospective randomized clinical trial. Knee Surg Sports Traumatol Arthrosc. 2016;24(7):2209-15.
-
43Coda RG, Cheema SG, Hermanns CA, et al. A Review of Online Rehabilitation Protocols Designated for Rotator Cuff Repairs. Arthrosc Sports Med Rehabil. 2020;2(3):e277-e288.
-
44Bakti N, Antonios T, Phadke A, Singh B. Early versus delayed mobilization following rotator cuff repair. J Clin Orthop Trauma. 2019;10(2):257-60.
-
45Li S, Sun H, Luo X, et al. The clinical effect of rehabilitation following arthroscopic rotator cuff repair: a meta-analysis of early versus delayed passive motion. Medicine (Baltimore). 2018;97(2):e9625.
-
46Mazzocca AD, Arciero RA, Shea KP, et al. The Effect of Early Range of Motion on Quality of Life, Clinical Outcome, and Repair Integrity After Arthroscopic Rotator Cuff Repair. Arthroscopy. 2017;33(6):1138-48.
-
47Hollman F, Wolterbeek N, Zijl JAC, van Egeraat SPM, Wessel RN. Abduction Brace Versus Antirotation Sling After Arthroscopic Cuff Repair: The Effects on Pain and Function. Arthroscopy. 2017;33(9):1618-26.
-
48Mahure SA, Rokito AS, Kwon YW. Transcutaneous electrical nerve stimulation for postoperative pain relief after arthroscopic rotator cuff repair: a prospective double-blinded randomized trial. J Shoulder Elbow Surg. 2017;26(9):1508-13.
-
49Moutzouros V, Jildeh TR, Khalil LS, et al. A Multimodal Protocol to Diminish Pain Following Common Orthopedic Sports Procedures: Can We Eliminate Postoperative Opioids? Arthroscopy. 2020;36(8):2249-57.
-
50Cohen DB, Kawamura S, Ehteshami JR, Rodeo SA. Indomethacin and celecoxib impair rotator cuff tendon-to-bone healing. Am J Sports Med. 2006;34(3):362-9.
-
51Virchenko O, Skoglund B, Aspenberg P. Parecoxib impairs early tendon repair but improves later remodeling. Am J Sports Med. 2004;32(7):1743-7.
-
52Oh JH, Seo HJ, Lee YH, Choi HY, Joung HY, Kim SH. Do Selective COX-2 Inhibitors Affect Pain Control and Healing After Arthroscopic Rotator Cuff Repair? A Preliminary Study. Am J Sports Med. 2018;46(3):679-86.
-
53Blomquist J, Solheim E, Liavaag S, Baste V, Havelin LI. Do nonsteroidal anti-inflammatory drugs affect the outcome of arthroscopic Bankart repair? Scand J Med Sci Sports. 2014;24(6):e510-4.
-
54Constantinescu DS, Campbell MP, Moatshe G, Vap AR. Effects of Perioperative Nonsteroidal Anti-inflammatory Drug Administration on Soft Tissue Healing: A Systematic Review of Clinical Outcomes After Sports Medicine Orthopaedic Surgery Procedures. Orthop J Sports Med. 2019;7(4):2325967119838873.
-
55Toma O, Persoons B, Pogatzki-Zahn E, Van de Velde M, Joshi GP; PROSPECT Working Group collaborators. PROSPECT guideline for rotator cuff repair surgery: systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia. 2019;74(10):1320-31.
-
56Garnaud B, Mares O, L’hermite J, et al. Multimodal oral analgesia strategy after ambulatory arthroscopic shoulder surgery: case series using adaptive therapeutic approaches by sequential analysis. J Shoulder Elbow Surg. 2021;30(2):250-7.
-
57An VVG, Farey JE, Karunaratne S, Smithers CJ, Petchell JF. Subacromial analgesia via continuous infusion catheter vs. placebo following arthroscopic shoulder surgery: a systematic review and meta-analysis of randomized trials. J Shoulder Elbow Surg. 2020;29(3):471-82.
-
58Ciccone WJ, Busey TD, Weinstein DM, Walden DL, Elias JJ. Assessment of pain relief provided by interscalene regional block and infusion pump after arthroscopic shoulder surgery. Arthroscopy. 2008;24(1):14-9.
-
59Laurila PA, Löppönen A, Kanga-Saarela T, Flinkkilä T, Salomäki TE. Interscalene brachial plexus block is superior to subacromial bursa block after arthroscopic shoulder surgery. Acta Anaesthesiol Scand. 2002;46(8):1031-6.
-
60Hansen BP, Beck CL, Beck EP, Townsley RW. Postarthroscopic glenohumeral chondrolysis. Am J Sports Med. 2007;35(10):1628-34.
-
61Fredrickson MJ, Krishnan S, Chen CY. Postoperative analgesia for shoulder surgery: a critical appraisal and review of current techniques. Anaesthesia. 2010;65(6):608-24.
-
62Cho NS, Ha JH, Rhee YG. Patient-controlled analgesia after arthroscopic rotator cuff repair: subacromial catheter versus intravenous injection. Am J Sports Med. 2007;35(1):75-9.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- The importance of pain control
- Learning from pain to make the patient feel better
- Perioperative pain management in arthroscopic surgery of the shoulder
- Perioperative pain management in arthroscopy of the elbow
- Perioperative analgesia in arthroscopic surgery of the wrist and hand
- Perioperative analgesia in arthroscopy of the hip
- Perioperative analgesia in arthroscopic surgery of the knee
- Perioperative pain management in arthroscopy of the ankle
- Postoperative neuropathic pain in traumatology
- Capsaicin 179 mg patch application technique
- Type 3 SLAP: bucket handle tear
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.