Perioperative pain management in arthroscopy of the ankle
Manejo perioperatorio del dolor en artroscopia de tobillo
Resumen:
Pese a existir menor evidencia que en otras articulaciones, el control del dolor postoperatorio en los procedimientos que implican una artroscopia de tobillo se ha visto relacionado con una menor estancia hospitalaria, un menor número de complicaciones y un mejor resultado quirúrgico en general, además de posibilitar que la mayor parte de estas cirugías se hagan en regímenes hospitalarios ambulatorios.
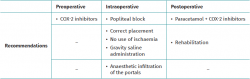
Se han descrito diversas estrategias para mejorar el control del dolor perioperatorio en las artroscopias de tobillo. La utilización de antiinflamatorios inhibidores de la COX-2, si bien con escasa evidencia, puede utilizarse si se prevé que la duración quirúrgica va a ser superior a 2 horas.
La analgesia multimodal ha demostrado mejorar el control del dolor posquirúrgico en las artroscopias de tobillo. La estrategia ideal consiste en una adecuada anestesia raquídea, combinada con un bloqueo poplíteo posterior sensitivo y simpático con ropivacaína 0,2% (20 mL), que permite el control analgésico hasta 12 horas tras la intervención (siendo el mayor pico de dolor tras la artroscopia de tobillo entre las horas sexta y duodécima postoperatorias).
La correcta posición del paciente, el tipo y el tiempo de isquemia empleados, la utilización de sistemas de lavado por gravedad y la infiltración posquirúrgica intraarticular a través de los portales con bupivacaína al 0,5% (20 mL) han demostrado mejorar el dolor posquirúrgico de los pacientes sometidos a procedimientos artroscópicos.
La analgesia combinada (paracetamol + antiinflamatorio no esteroideo clásico o inhibidor selectivo de la COX-2) es la preferida para un mejor control en el postoperatorio, principalmente cuando ceden los efectos del bloqueo. La rehabilitación, asimismo, en forma de fisioterapia, hidroterapia o electroterapia, puede jugar un papel importante en función de la patología intervenida por artroscopia.
Abstract:
Despite the existence of a lesser body of evidence than in other joints, the control of postoperative pain in ankle arthroscopy has been associated to shorter hospital stay, fewer complications and a better surgical outcome in general, and moreover makes it possible to perform most such surgeries on a hospital ambulatory basis.
Different strategies have been described to improve perioperative pain control in ankle arthroscopy. Although based on little evidence, the use of COX-2 inhibiting anti-inflammatory drugs may be indicated if surgery is expected to last for over two hours.
Multimodal analgesia has been shown to improve postoperative pain control in ankle arthroscopy. The ideal strategy comprises adequate spinal anaesthesia, combined with sympathetic and sensory posterior popliteal block with 0.2% ropivacaine (20 ml), which affords pain control for up to 12 hours after the operation (peak pain following ankle arthroscopy manifesting between 6-12 hours after surgery).
Correct positioning of the patient, adequate type and time of ischaemia, the utilisation of gravity lavage systems, and postoperative intraarticular infiltration through the portals with 0.5% bupivacaine (20 ml) have been shown to improve postoperative pain in patients subjected to arthroscopic procedures.
Combined analgesia (paracetamol plus a classical non-steroidal anti-inflammatory drug or selective COX-2 inhibitor) is the preferred option for improved control in the postoperative period, mainly once the effects of block subside. Likewise, rehabilitation in the form of physiotherapy, hydrotherapy or electrotherapy may play an important role, depending on the disease condition for which arthroscopy is performed.
Introduction
Arthroscopy of the ankle is increasingly used for the diagnosis and treatment of disorders of this anatomical region. Improved surgical techniques have made it possible to expand the indications of this procedure, including the management of instability (lateral and medial), impingement, osteochondritis dissecans, osteochondral lesions, assistance in ankle arthrodesis and fractures, arthrofibrosis, synovitis, osteoarthritis (including septic arthritis) and free bodies(1,2) (anterior chamber). Likewise, it is possible to treat disorders related to os trigonum, frictional syndromes, posterior arthrofibrosis, tendon transpositions and assistance in subtalar and tibioastragaline arthrodesis(3,4) (posterior chamber).
The management of postoperative pain in ankle surgery is crucial for patient comfort and to allow early mobilisation of the joint — though no consensus has been established to date regarding the protocols for these procedures(5). In general, arthroscopy of the ankle is able to reduce complications and hospital stay compared with open surgery performed with the same indication(1,5). Nevertheless, different procedures have been described that can help to deal with pain following arthroscopy of the ankle. Traditionally, management focused on analgesia upon demand, in accordance with the patient needs. This was subsequently followed by more protocolised analgesia regimens during the first 24 hours postsurgery. At present, the possibility of using popliteal blocks, intraarticular anaesthetic infiltration through the portals at the end of surgery, multimodal analgesia and postoperative rehabilitation appear to improve pain control, though with important variations depending on the type of arthroscopic procedure performed, since the latter may range from the simple dissection of an anterolateral impingement to arthroscopy-assisted arthrodesis.
The present review reflects the available evidence on perioperative analgesia in arthroscopy of the ankle, and seeks to offer a series of recommendations in this regard.
Importance of perioperative pain in arthroscopic surgery of the ankle
Although dependent upon the procedure involved, postoperative pain following arthroscopy of the ankle generally reaches maximum intensity between 6-12 hours after completion of the procedure(6), and remains relatively intense until 24 hours postsurgery, after which it gradually decreases. Tissue injury caused by arthroscopic surgical procedures stimulates the free nerve endings and afferent nociceptors. This enhanced activity is further incremented by the effects of tissue inflammation factors such as bradykinin, histamine and serotonin, which are released by the damaged cells. In addition to direct stimulation, these neuroactive peptides act together with the prostaglandins (particularly prostaglandin E2, derived from arachidonic acid) to sensitise the peripheral primary nociceptive afferents, reducing their activation threshold and shortening their latency of response — with alteration of the central processing of sensory stimuli, facilitating nociceptive transmission in the dorsal horn of the spinal cord(7). Such sensitisation is considered to be the neurophysiological basis not only of common postoperative pain but also of exaggerated pain sensation clinically characterised by hyperalgesia — a state of increased sensitivity to stimuli that are painful under normal conditions — and allodynia — pain sensation produced by normally harmless stimuli such as light palpation. Although the effect of sustained nociceptive activity is essential for establishing primary hyperalgesia, the actions of the tissue mediators of pain and inflammation are diffuse and not limited to the area of initial pain projection — the pain spreading through secondary hyperalgesia, affecting areas at a distance from the skin incision(7).
The importance of this is that if the initial postoperative peak in pain intensity can be reduced, most patients can be discharged in the first 24 hours; this in turn would allow many surgeries to be performed on an ambulatory basis or with minimum stay, and rehabilitation could be started early if needed — thus influencing the final functional outcome of the patient(8,9).
However, as mentioned above, patient pain is not only dependent upon whether surgery is arthroscopic or not, but also on the surgical procedure itself. Arthroscopic surgery of the ankle normally minimises soft tissue damage and allows faster and less painful recovery than open surgery(8). Therefore, the use of arthroscopy in itself generally implies better functional recovery in ankle surgeries. If we further add pain control to the arthroscopic procedure, most surgeries can be performed on an ambulatory basis or with short patient admission(10).
Although very little literature is available on the issue, those procedures that invade joint cartilage (debridement or abrasion of osteochondral lesions, curettage for arthrodesis) are the most painful during the postoperative period. In addition, mention also must be made of the duration of arthroscopy (with pain being greater in procedures lasting over two hours), the use of ischaemia, and saline (cleansing) infusion with pump systems(11). Other patient-dependent factors such as the female sex and prior anxiety or depression — studied in other joints — have not yet been correlated in ankle surgery(12).
Assessment of pain in arthroscopic surgery of the ankle
The measurement of outcomes has been widely used in orthopaedic surgery. In the past, the assessment of outcomes was only based on the clinical results reported by the surgeon. However, in the last decade, instruments developed and validated according to the feedback provided by the patients have been gradually introduced. In this regard, we now have instruments for measuring the impact of our interventions upon patient health, as well as specific criteria for knowing the outcome in each of the anatomical regions(12).
Many specific questionnaires for the anatomical area of the ankle and foot are available. That of the American Orthopaedic Foot and Ankle Society (AOFAS) is one of the most widely used instruments. This scale assesses three fundamental aspects related to the foot and ankle, namely pain, function and alignment. Based on this scale, with a theoretical score of 100, pain yields a score ranging from up to 40 if the patient has no discomfort of any kind to 0 points in the case of continuous severe pain. The AOFAS scale has not been validated in Spanish, and studies on its consistency are lacking(13). There are other scales such as the Foot and Ankle Ability Measure (FAAM), which is a questionnaire with 29 sections, divided into 21 addressing daily life and 8 referred to sports activity — though this instrument likewise has not been validated in Spanish(14). In turn, the Manchester-Oxford Foot Questionnaire (MOXFQ) comprises 16 sections initially addressing hallux valgus surgery, though it has since been extended to the rest of foot and ankle disorders. In contrast to the above-mentioned scales, this instrument has been validated in Spanish (Spanish Manchester-Oxford Foot Questionnaire)(15). Another important scale is the Foot Function Index (FFI)(16), subdivided into three sections (pain, disability and limitation of activity). This scale was initially developed for patients with rheumatoid arthritis, though it has been extended to all foot and ankle conditions, including the postoperative period.
Despite the existence of all the above scales, the visual analogue scale (VAS) remains the first choice for assessing postoperative pain in surgery of the foot and ankle. In this regard, a specific VAS for foot and ankle disease has been developed — the so-called Visual-Analogue-Scale Foot and Ankle (VAS-FA)(17). This is a questionnaire with 20 questions divided into three categories: pain (4), function (11) and other complaints (5). Each question has a score from 0-100; the total score can therefore range from 0-2000. The score obtained is divided by 20 to obtain a final value between 0 (maximum pain and poorest function) and 100 (no pain and with full function). This questionnaire was developed in the United States and has been validated in Europe(17).
Preoperative management
Preventive analgesia consists of starting treatment before the onset of surgical pain, in order to avoid peripheral and central sensitisation. Many studies have explored this concept, though most of them lack consistency; this topic is therefore currently the subject of debate(18,19). The concept of preventive analgesia has gradually given way to that of multimodal analgesia, which seeks to improve postoperative pain by combining various pharmacological and non-pharmacological tools.
The literature on multimodal analgesia in foot and ankle surgery in general, and in arthroscopic surgery in particular, is very limited. Michelson et al.(20) initially proposed a treatment for arthrodesis of the ankle and hindfoot, consisting of the preoperative administration of oxycodone (10 mg), celecoxib (200 mg), pregabalin (75 mg), paracetamol (1 g) and prednisone (40 mg). The results obtained were favourable. However, doubts were expressed about the need for this protocol in less invasive surgery, such as arthroscopy, where the lesser tissue aggression involved would allow the use of lower-step analgesic measures with fewer side effects(20).
Several studies have analysed the use of preoperative analgesic regimens based on non-opioid drugs such as selective COX-2 inhibitors (parecoxib) or corticosteroids (prednisone)(20), without being able to recommend their systematic use — though they could be indicated in arthroscopic surgeries lasting over two hours.
Intraarticular infiltration anaesthesia has indeed been shown to reduce pain during the immediate postoperative period, together with block procedures. However, this strategy is nowadays more systematically used at the end of the arthroscopic procedure; as a result, it likewise presently cannot be recommended before surgery(21).
In contrast to other anatomical regions such as the shoulder or knee, there is currently not enough evidence to recommend the preoperative use of COX-2 inhibiting non-steroidal anti-inflammatory drugs (NSAIDs) in arthroscopy of the ankle. Nevertheless, in prolonged arthroscopic surgeries or patients with arthritic disorders, the use of combinations of paracetamol (1 g) with celecoxib (200 mg) and pregabalin (75 mg) has been proposed — here again with little evidence in arthroscopic surgery and with somewhat greater evidence in more aggressive and longer-lasting surgeries(21).
Intraoperative management
Arthroscopy of the ankle traditionally has been performed under spinal anaesthesia, except in cases of long surgeries, where general anaesthesia has been preferred. However, the possibility of combining an epidural catheter has popularised spinal anaesthesia in surgeries of this kind(22).
Another possibility is to achieve complete sensory and motor block of the ankle without having to resort to general or spinal anaesthesia for the operation. In order to do this, complete sciatic nerve block would be required at the level of the popliteal space, using high concentration (0.75%) ropivacaine mixed with some short-latency anaesthetic (mepivacaine or lidocaine at a concentration of 2%). In addition to sciatic nerve block, we also would have to block the saphenous nerve, since it innervates the entire medial zone of the ankle-foot. This nerve can be blocked at proximal level (it is a branch of the femoral nerve) or at the knee (in proximity to the vein)(23,24).
The inconvenience of the mentioned complete block (motor and sensory) is the use of the ischaemia cuff. The latter is placed on the thigh — a zone where the patient would not be anaesthetised with this type of block. To solve this problem, sciatic nerve block should be performed practically at subgluteal level, adding a proximal femoral block to thus cover the entire surgical zone, including the region on which the ischaemia cuff is placed — since only the lateral femorocutaneous and major and minor obturator nerves (not needed) would remain without anaesthetic block(23,24,25).
This complete motor block offers the advantage that its effect persists over time during the postoperative period, allowing control of the immediate postoperative pain of the patient(20). Nevertheless, its action is brief, and the effect subsides 2-3 hours after the operation. It therefore would not be possible to control the maximum peak in pain that occurs 6-12 hours after the arthroscopy procedure(23,24,25).
In relation to surgery itself, a number of aspects should be taken into account with the aim of reducing postoperative pain:
- Duration of the operation: patients undergoing arthroscopy with a duration of under two hours experience less postoperative pain than those in which the surgery time is longer(21).
- Use of the ischaemia cuff (tourniquet): traditionally, a higher level of postoperative pain has been observed in patients subjected to arthroscopy of the ankle with the application of ischaemia as a method to better visualise the joint. This affirmation has currently been questioned, though there is evidence in favour of not using ischaemia in arthroscopy of the ankle, as the results obtained are similar to those cases where the tourniquet was applied, and without the potential complications of its use (neurological complications, soft tissue damage, postoperative pain)(26,27). If ischaemia is indeed used, it should be brief (under two hours) and of low pressure (250 mmHg)(1).
- Distraction systems: up until a few years ago, active distraction was used to achieve better visualisation of the tibioastragaline joint. The current tendency is to use the dorsiflexion system to avoid excessive distraction of the joint, which could increase ankle pressure and the pain experienced by the patient during the immediate postoperative period, as well as the neurological damage due to the traction system itself. There are studies indicating that the combined use of an ischaemia tourniquet and an active distraction system produces greater ankle pressure that can cause soft tissue damage and therefore greater postoperative pain(28).
- Patient positioning: supine decubitus (simply on the surgical table or on a leg support, so that the ankle falls by gravity) is the position of choice for operating upon the anterior chamber, while prone decubitus is the choice for the posterior chamber. Likewise, patient positioning in lateral decubitus has been described for dual-chamber surgery(1). However, this latter position has been associated with greater technical difficulties in gaining access to the chambers, with a greater risk of neurological damage and of consequent postoperative neuropathic pain. The bone surfaces should be cushioned and protected, particularly in lateral decubitus (hip and contralateral knee), in order to minimise postoperative pain and possible neurological damage(1).
- Use of a pump or gravity saline system: both options are valid and can be used in arthroscopy of the ankle. However, the pump system increases the risk of fluid extravasation towards the surrounding tissues, which can result in increased compartmental pressure and ischaemia(1), with an increase in postoperative pain.
- Neurological damage: this is the main complication of arthroscopy of the ankle. In the anterior chamber, mention must be made of damage to the superficial peroneal nerve (fundamentally its lateral dorsal cutaneous branch), while in the posterior chamber damage to the sural nerve stands out. Both situations cause neuropathic pain in the postoperative period, which is mostly reversible over time. The control of neurological damage during the operation is essential in order to avoid postoperative neuropathic pain. In the anterior chamber, it is advisable to visualise the superficial peroneal nerve branches with the ankle in plantar flexion and inversion, performing the mark at that site. Once the ankle returns to its neutral position, the nerve displaces laterally(29); the safe place for the anterolateral portal is therefore just medial to the mentioned mark(1). In the posterior chamber, and in order to minimise the risk of neurological damage, Van Dijk et al.(30) recommend placing the posterolateral portal at the level of, or slightly above, the tip of the lateral malleolus, adjacent to the Achilles tendon. In this way we minimise the possible risk of damage to the sural nerve, which is described crossing the lateral margin of the Achilles tendon subcutaneously, with an average of 9.8 cm (range: 6.5 to 16 cm) proximal to the insertion of the Achilles tendon.
Postoperative management
Postoperative block, together with intraarticular anaesthetic injection, have been shown to markedly reduce postoperative pain — both techniques currently being regarded as the options of choice(1).
In relation to block, the effect is fundamentally sensory; as a result, the patient is able to move the extremity, which is useful not only for recovery but also for assessing possible damage (neurological and tendinous) occurring during surgery. The classical technique consists of sciatic block at popliteal level — the preferred approach being ultrasound-guided block for greater safety and efficacy, using a 10 MHz linear probe and a Vygon® plexus needle (100 mm). Ropivacaine should preferably be used, due to its longer lasting effect, at a concentration of 0-2% (20 ml). Ideally, the division of the sciatic nerve at popliteal level should be visualised by ultrasound in order to be sure that both are blocked (internal and external popliteal sciatic nerves). This block affords adequate pain control for 12-15 hours(31). It should be remembered that it is precisely after 6-12 hours when peak pain manifests following arthroscopy of the ankle. This type of block is therefore especially indicated and useful, independently of whether general or epidural anaesthesia has been performed.
With regard to intraarticular drug injection after arthroscopy of the ankle, Rasmussen and Kehlet(32) were the first to demonstrate its usefulness, administering a formulation of bupivacaine, morphine and methylprednisolone that demonstrated superiority versus placebo. However, this combination generated much controversy due to the use of corticosteroids (one of the patients developed septic arthritis) and an opiate; more conservative alternatives were therefore explored. In this context, Middleton et al.(33) recorded good results with an isolated injection of 20 ml of 0.5% bupivacaine versus placebo — the difference being more notorious 12 hours after arthroscopy (as assessed by the VAS scale). Moreover, the patients in the placebo group required more rescue analgesia during the first 24 hours. These findings were subsequently reproduced, likewise drawing favourable conclusions regarding the use of 0.5% bupivacaine(34).
During the postoperative period of arthroscopy of the ankle, the combined analgesia treatments have been found to be the techniques affording greater effectiveness in dealing with pain. The best results are obtained using the combination of paracetamol (1 g) with anti-inflammatory drugs, including classical NSAIDs (diclofenac, ibuprofen) or selective COX-2 inhibitors (etoricoxib, celecoxib)(21). This combination has evidenced greater pain control versus both medications administered separately. The administration of combination treatments with gabapentin (300 mg every 12 hours) and celecoxib (200 mg every 12 hours) has also been shown to be effective in managing postoperative pain(21,35).
Rehabilitation has been shown to improve the outcomes of arthroscopy of the ankle, though it has been individualised according to the type of lesion subjected to surgery, i.e. there is no specific postoperative rehabilitation protocol, and the approach depends on the disease condition for which the patient has been operated upon. In rehabilitation following ligament repair, work upon proprioception is particularly important during the first weeks in which loading is tolerated(36). Cryotherapy may be indicated in the first hours after arthroscopy to reduce local metabolism and thus the inflammation and pain. Passive, active and forced kinesitherapy techniques are indicated in conditions predominantly characterised by stiffness, such as arthrofibrosis, where arthroscopic arthrolysis is performed. Hydrotherapy(37) is an option in arthroscopic surgery for fractures, instability or with the development of complications such as Südeck syndrome (more common in procedures involving the anterior chamber than the posterior chamber). Electrostimulation appears to be useful in the case of recovery from ankle fractures(38). Lastly, spectrotherapy is useful in all patients that develop painful muscle contractures, chronic joint inflammation and degenerative arthropathies in which arthroscopy plays a palliative role consisting of debridement, cleaning of the joint and the removal of free bodies(7) (Table 1).
Conclusions
The existing literature is too limited to allow firm conclusions to be drawn regarding the perioperative management of ankle pain in arthroscopic procedures. The preoperative administration of COX-2 inhibitors may be indicated in ankle arthroscopy procedures lasting over two hours (little evidence). Surgery without ischaemia, using gravity lavage and intraarticular infiltration of the portals with bupivacaine at the end of the procedure reduces postoperative pain. Postsurgical popliteal sensory and sympathetic block is the technique of choice and allows the control of peak pain sensation in the immediate postoperative period. Multimodal analgesia with the use of paracetamol and selective COX-2 inhibitors offers better pain control than each analgesic administered separately, during the first postoperative days.
Información del artículo
Cita bibliográfica
Autores
Alejandro Lorente Gómez
Departamento de Traumatología y Cirugía Ortopédica Hospital Universitario Ramón y Cajal, Madrid
Hospital Universitario HM Sanchinarro. Madrid
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Epstein D, Black B, Sherman S. Anterior Ankle Arthroscopy. Indications, pitfalls, and complications. Foot Ankle Clin. 2015;20:41-57.
-
2Blázquez M, Iglesias Durán E, San Miguel Campos M. Complicaciones tras la artroscopia de tobillo y retropié. Rev Esp Cir Ortop Traumatol. 2016;60:387-93.
-
3Amendola A, Lee KB, Saltzman CL, Suh JS. Technique and early experience with posterior arthroscopic subtalar arthrodesis. Foot Ankle Int. 2007;28:298-302.
-
4Amendola A, Bonasia DE. When is ankle arthroscopy indicated in ankle instability? Oper Tech Sports Med. 2010;18:2-10.
-
5Perera A. Advances in minimally invasive surgery of the foot and ankle-percutaneous, arthroscopic, and endoscopic operative techniques. Foot Ankle Clin. 2016;21:13-4.
-
6Zekry M, Shahban SA, EL Gamal T, et al. A literature review of the complications following anterior and posterior ankle arthroscopy. Foot Ankle Surg. 2019;25:553-8.
-
7Elmlund A, Winson I. Arthroscopic ankle arthrodesis. Foot Ankle Clin. 2015;20:71-80.
-
8An M, Su X, Wei M, et al. Local anesthesia combines with intraarticular ropivacaine con provide satisfactory pain control in ankle arthroscopic surgery: a retrospective cohort study. J Orthop Surg. 2020;28:1-8.
-
9Miller & Cole. Artroscopia. Ed. Marbán; 2011.
-
10Yáñez-Arauz JM, Raimondi N, Tomé C, et al. Complicaciones en la artroscopia posterior de tobillo por portales clásicos y sin distracción. Acta Ortop Mex. 2021;35:46-50.
-
11Strube P, Schöpe T, Hölzl A, et al. Influence of Anxiety and Depression, Self-Rated Return-to-Work Problems, and Unemployment on the Outcome of Outpatient Rehabilitation After Shoulder Arthroscopy. Am J Phys Med Rehabil. 2019;98:1118-24.
-
12Castellet Feliu E, Vidal N, Conesa X. Escalas de valoración en cirugía ortopédica y traumatología. Fundación Mapfre Trauma. 2010;21(Supl).
-
13Ponkilainen VT, Uimonen M, Repo JR, et al. Validity and internal consistency of the American Orthopaedic Foot and Ankle Society Midfoot Scale in patients with Lisfranc injury. Foot Ankle Surg. 2020;26(5):523-9.
-
14Hoch J, Powden C, Hoch M. Reliability, minimal detectable chane and responsiveness of the Quick-FAAM. Phys Ther Sport. 2018;32:269-72.
-
15Garcés JB, Winson I, Godhahn S, et al. Reliability, validity and responsiveness of the Spanish Manchester-Oxford Foot Questionnaire (MOXFQ) in patients with foot or ankle surgery. Foot Ankle Surg. 2016;22:59-70.
-
16Budiman-Mak E, Conrad KJ, Roach KE. The Foot Function Index: a measure of foot pain and disability. J Clin Epidemiol. 1991;44:561-70.
-
17Saarinen AJ, Uimonen MM, Sandelin H, et al. Minimal important change for the visual analogue scale foot and ankle (VAS-FA). Foot Ankle Surg. 2021;27:196-200.
-
18Cousins MJ. Prevention of postoperative pain. Proceedings of the Fifth World Conrgess on Pain. Elsevier Science Publishers; 1991. pp. 41-57.
-
19Kehlet H, Dahl JB. The value of multimodal or balanced analgesia in postoperative pain treatment. Anesth Anal. 1993;77:1048-56.
-
20Michelson JD, Addante RA. Charlson MD. Multimodal analgesia therapy reduces length of hospitalization in patients undergoing fusions of the ankle and hindfoot. Foot Ankle Int. 2013;34:1526-34.
-
21Kohring J, Orgain N. Multimodal analgesia in Foot and Ankle surgery. Orthop Clin North Am. 2017;48:495-505.
-
22Reilley T, Gerhardt M. Anesthesia for foot and ankle surgery. Clin Podiart Med Surg. 2002;19:125-47.
-
23Vadivelu N, Kai A, Maslin B, et al. Role of regional anesthesia in foot and ankle surgery. Foot Ankle Spec. 2015;8:212-9.
-
24Pearce C, Hamilton P. Current concepts review: regional anesthesia for foot and ankle surgery. Foot Ankle Int. 2010;31:732-9.
-
25Sagherian B, Kile T, Seamans D, et al. Lateral popliteal block in foot and ankle surgery: comparing ultrasound guidance to nerve stimulation. A prospective randomized trial. Foot Ankle Surg. 2021;27:175-80.
-
26Dimnjakovic D, Hrabac P, Bojanic I, et al. Value of tourniquet use in anterior ankle arthroscopy: a randomized controlled trial. Foot Ankle Int. 2017;38:716-22.
-
27Zaidi R, Hasan K, Sharma A, et al. Ankle arthroscopy: a study of tourniquet versus no tourniquet. Foot Ankle Int. 2014;35:478-82.
-
28Ahn JH, Park D, Park YT, et al. What should we be careful of ankle arthroscopy. Orthop Surg (Hong Kong). 2019;27:1-9.
-
29De Leeuw PA, Golano P, Blankevoort L, et al. Identification of the superficial peroneal nerve: anatomical study with surgical implications. Knee Sports Traumatol Arthrosc. 2016;24:1381-5.
-
30Van Dijk CN, Scholten PE, Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16:871-6.
-
31Christiansen CB, Madsen MH, Rothe C. Volume of ropivacaine 0.2% and sciatic nerve block duration: a randomized, blinded trial in healthy volunteers. Acta Anaesthesiol Scand. 2020;64:238-44.
-
32Rasmussen S, Kehlet H. Intrarticular glucocorticoid, morphine and bupivacaine reduces pain and convalescence after arthroscopic ankle surgery: a randomized study of 36 patients. Acta Orthop Scan. 2000;71:301-4.
-
33Middleton F, Coakes J, Umarji S, et al. The efficacy of intra-articular bupivacaine of relief of pain following arthroscopy of the ankle. J Bone Joint Surg Br. 2006;88:1603-5.
-
34Liszka H, Gadek A. Preemptive local anesthesia in ankle arthroscopy. Foot Ankle Int. 2016;37:1326-32.
-
35Ong CK, Seymour RA, Lirk P, et al. Combining paracetamol (acetaminophen) with nonsteroidal antiinflammatory drugs: a qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg. 2010;110:1170-9.
-
36Shawen S, Dworak T, Anderson R. Return to play following ankle sprain and lateral ligament reconstruction. Clin Sports Med. 2016;35:697-709.
-
37Cuesta-Barriuso R, Gómez-Conesa A, López-Pina JA. Physiotherapy treatment in patients with hemophilia and chronic ankle arthropathy: a systematic review. Rehabil Res Pract. 2013;2013:30524.
-
38Lin CW, Donkers NAJ, Refshauge KM, et al. Rehabilitation for ankle fractures in adults. Cochrane Database Syst Rev. 2012;11:CD005595.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- The importance of pain control
- Learning from pain to make the patient feel better
- Perioperative pain management in arthroscopic surgery of the shoulder
- Perioperative pain management in arthroscopy of the elbow
- Perioperative analgesia in arthroscopic surgery of the wrist and hand
- Perioperative analgesia in arthroscopy of the hip
- Perioperative analgesia in arthroscopic surgery of the knee
- Perioperative pain management in arthroscopy of the ankle
- Postoperative neuropathic pain in traumatology
- Capsaicin 179 mg patch application technique
- Type 3 SLAP: bucket handle tear
Más en PUBMED
Más en Google Scholar


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.