Perioperative analgesia in arthroscopy of the hip
Analgesia perioperatoria en artroscopia de cadera
Resumen:
El número de artroscopias de cadera ha aumentado de manera exponencial en los últimos 15 años. El control del dolor perioperatorio tras el procedimiento es fundamental para una adecuada satisfacción del paciente con su cirugía y una buena evolución del proceso. Sin embargo, no existe un consenso en cuanto a la pauta más adecuada de tratamiento.
El dolor tras una artroscopia de cadera está condicionado por factores físicos dependientes de la cirugía, como el tiempo de tracción, la presión de la bomba, la extravasación de líquido a otros tejidos o el tipo de procedimientos que se lleven a cabo, y por otros más difíciles de controlar, dependientes del paciente, como el perfil psicológico o la tolerancia individual al dolor.
Es indiscutible que el abordaje multimodal es el camino más adecuado para el correcto control del dolor perioperatorio en la artroscopia de cadera, que conlleva la disminución del uso de analgésicos opiáceos y sus efectos secundarios en el postoperatorio inmediato, la movilización precoz del paciente, la disminución de tiempo en la sala de recuperación posquirúrgica y la estancia hospitalaria, lo que supone un mayor confort del paciente.
Las pautas principales de este abordaje multimodal son una adecuada analgesia preoperatoria mediante la administración de antiinflamatorios no esteroideos 1 hora antes de la cirugía, una correcta analgesia postoperatoria, basada fundamentalmente en la analgesia farmacológica, en las infiltraciones locales pericapsulares, periacetabulares y de los portales utilizados durante la cirugía, así como en los bloqueos nerviosos y, por último, una adecuada analgesia postoperatoria, fundamentalmente farmacológica.
Abstract:
The number of hip arthroscopies has grown exponentially in the last 15 years. Perioperative pain control is very important for adequate patient satisfaction with surgery and for a correct evolution of the process. However, there is no consensus regarding the management strategy of choice.
Pain following arthroscopy of the hip is conditioned by physical factors related to surgery, such as traction time, pump pressure, fluid extravasation towards other tissues, or the type of procedures performed, as well as by other factors that are patient-dependent and more difficult to control, such as the psychological profile or individual tolerance of pain.
A multimodal approach is clearly the best way to secure correct control of perioperative pain in arthroscopy of the hip, affording a decrease in opioid analgesic use and the associated side effects in the immediate postoperative period, early patient mobilisation, and a reduction of stay in the postsurgery recovery room and in hospital — all of which contributes to improve patient comfort.
The main elements of this multimodal approach are adequate preoperative analgesia administering non-steroidal anti-inflammatory drugs one hour before surgery, correct postoperative analgesia based fundamentally upon pharmacological agents, pericapsular and periacetabular local infiltrations, as well as infiltrations of the portals used during surgery, nerve blocks and finally adequate postoperative analgesia based mainly on the administration of drugs.
Introduction
Arthroscopy of the hip has grown exponentially in recent years. In England alone, the growth has been 723% in the last decade, and this figure is expected to reach 1,388% by 2023(1). Adequate postoperative pain control is crucial for improving patient satisfaction with surgery, and facilitates early mobilisation as well as the prompt start of rehabilitation(2,3). Development and improvement of the technique have made it possible to increase the number of cases in which it is carried out on an ambulatory basis. Both the percentage of patient discharge from hospital and readmission are conditioned by the management of postoperative pain. Inadequate pain management leads to delays in recovery, adverse psychological effects and an increased risk of developing chronic pain associated to the process(2). However, there is no standardised protocol for the management of perioperative pain in this surgical procedure.
The postoperative pain experienced by the patient following arthroscopy of the hip is due to a number of factors:
- Factors dependent upon the surgical technique, such as leg traction, capsule distension or fluid extravasation towards the surrounding tissues(4).
- Factors dependent upon the patient disease condition and the possible postoperative complications.
- Factors related to the psychological profile of the patient and his or her tolerance of pain(1). The presence of psychiatric disorders in patients subjected to arthroscopy of the hip due to femoroacetabular impingement appears to be quite common(5). As in other disease conditions, it is known that this can worsen the surgical outcome(6). However, there have also been promising publications in this regard, as in the study published by Zacharias(7), who recorded a decrease in psychiatric medication use in patients diagnosed with depression or anxiety at least one year before surgery.
Some intraoperative manoeuvres, such as the use of high pressures in the pump, labral repair and femoral osteochondroplasty appear to cause more pain during the postoperative phase. Utilisation of the fluid infusion pump at a pressure of 40 mmHg may result in less postoperative pain(8).
The combination of correct pre- and postoperative analgesic medication with nerve blocks appears to offer the best postoperative analgesia, reducing morphic drug use in the first hours after surgery — though the side effects of each option need to be taken into account(9,10).
Assessment of postoperative pain in arthroscopy of the hip
The assessment of postoperative pain in arthroscopy of the hip is mainly based on the visual analogue scale (VAS), since this tool is simple and easy for the patient to understand. The assessment scales specifically designed for application with arthroscopy of the hip are not useful for this assessment in question, since they do not address immediate postoperative pain but are focused on follow-up at least one month after surgery.
Another parameter often used in the literature to assess the efficacy of pain treatment in the immediate postoperative period is the reduction of opioid use in the first hours after surgery.
Preoperative pain control
The concept of preventive analgesia is increasingly important in the multimodal management of pain in surgery.
It seems that a single dose of non-steroidal anti-inflammatory drugs (NSAIDs) can reduce postoperative pain and the need for opioids in the immediate postoperative period(11,12,13). Many of the studies found in the literature use 200 or 400 mg of celecoxib one hour before surgery. In the study on the triple-phase multimodal management of pain in arthroscopy of the hip published by Kolackzko et al., the first phase comprised the administration of a single preoperative dose of 975 mg of paracetamol, 300 mg of gabapentin and 200 mg of celecoxib(3).
A very interesting study carried out by Flavio García et al. on routine practices in arthroscopy of the hip among orthopaedic surgeons in different countries evidenced the differences found in the diverse geographical settings. According to the results obtained, preventive analgesia is not commonly used by 41.3% of the surgeons. Those who do use such analgesia prescribe NSAIDs, non-opiate analgesics such as paracetamol or salicylates. In geographical terms, 68.2% of the North American surgeons prescribe preventive analgesia, versus 29.5% in Central and South America, 27.3% of the surgeons in Europe, and 23.2% of those in Asia(2). As can be seen from the findings, North American surgeons are very much aware of the importance of this measure, while in Europe — and certainly also in Spain — this is not yet so.
In our opinion, it would be of benefit to introduce preventive analgesia in our practice.
Intraoperative pain control
The type of anaesthesia used during surgery influences intra- and postoperative pain control. In this respect, the use of general anaesthesia allows for greater patient comfort and control of muscle relaxation. This is important in view of its relation to the traction force needed to distract the joint and the potential complications associated with excessive traction in order to obtain sufficient space to correctly perform the required surgery. Other important factors are the pump operating pressure and the surgery time. The greater the pressure and the longer the time, the greater the probability of fluid extravasation towards the surrounding tissues and even into the abdominal cavity. Tissue distension can cause pain, and extravasation into the abdominal cavity may even produce compression and damage to nerve structures such as the crural nerve, and generate more pain in the postoperative period(4). Neuraxial anaesthesia affords more effective postoperative analgesia, but may have other undesired effects such as delayed complete clearance of the drug, which can cause falls, and the prolongation of hospital stay — this being particularly important in processes that can be carried out on an ambulatory basis(14).
In the context of multimodal management of postoperative pain in an arthroscopy of the hip, nerve blocks, particularly peripheral nerve block, seek to ensure adequate pain control in the immediate postoperative period, attempting to reduce the use of opioid analgesics and their side effects. The nausea or vomiting induced by these drugs is a frequent cause of delay in patient discharge from the postoperative recovery room and even in discharge from hospital in the case of surgery performed on an ambulatory basis(15,16).
Nerve blocks are mostly performed immediately before anaesthesia.
The hip joint is innervated by multiple nerves, and nerve block of the entire joint is therefore complex. The anterior portion of the capsule is innervated by the obturator and femoral nerves, which fundamentally receive information from that region, thereby leaving a between-nerves plane in part of the anterosuperior quadrant. The posterior portion of the capsule in turn is innervated by articular branches of the sciatic nerve, the superior gluteal nerve, the muscular branch innervating the quadratus femoris, and the inferior gluteal nerve(1,17,18). The first two cover the posterosuperior quadrant while the last two innervate the posteroinferior quadrant. This anatomical complexity makes it very difficult to achieve complete analgesic block of the hip, since doing so would require effective block of all these nerves as well as of the lateral femoral cutaneous nerve, implicated in innervation of the skin in the area where most of the hip arthroscopy portals are located.
The interesting anatomical study carried out by Mehewx showed the largest number of mechanoreceptors and sensory fibres to be located in the superolateral portion of the capsule, followed by its anterior zone — these regions coinciding with an important percentage of the disease conditions treated by means of hip arthroscopy. However, no sensory fibres were found in the inferior or posterior portion of the capsule(19).
The most frequently described blocks are femoral nerve block, lumbar plexus block and fascia iliaca block — though there is no clear preference for one specific technique. In fact, at present there is considerable controversy regarding their use.
Femoral nerve and lumbar plexus blocks afford good pain control, but also increase certain complications — particularly a risk of falls due to the motor block, especially of the quadriceps.
A number of studies involving block procedures that include the femoral nerve have reported improvement of pain in the immediate postoperative period, with a reduction of opiate use during the same period(20,21,22) in some of them, but also with a variable percentage of quadriceps weakness as well as falls attributable to motor block of this muscle(22,23). Falls of this kind can have important consequences, such as subcapital fracture due to neck weakness following resection of a cam-type deformity(24). In fact, some studies directly disadvise blocks of this kind, on the grounds that they do not afford better analgesia than other therapies, and moreover increase the risk of complications(25,26).
Fascia iliaca block does not appear to produce the same levels of analgesia and poses an increased risk of sensory neurological damage — especially of the lateral femoral cutaneous nerve(10). If obturator nerve block is added to fascia iliaca block, the analgesia achieved improves considerably(27).
Lumbar plexus block appears to offer better analgesia than fascia iliaca block, though in addition to falls(28), it may give rise to other undesired effects secondary to penetration of the neuraxial drug into the nervous system(28,29). In any case, there is considerable variability in the different publications.
The most recent studies describe spinal erector muscle blocks(30) involving infiltration of the lateral margins of the third lumbar spinous process. Zimmerer(30) recorded improved pain control versus placebo infiltration in the first 24 hours after surgery, though opiate use in the postoperative recovery room did not decrease. Descriptions have also been made of quadratus lumborum block, which has been used for years in abdominal surgery. This technique is performed in the anterolateral portion of the fascia of the quadratus lumborum muscle, and appears to reduce opiate use in the immediate postoperative period compared with patients in which no such block is performed(31).
In the study published by Kolackzko et al., the first phase involves the administration of preoperative analgesia as a single dose, as has been described above. Then, nerve block is performed in the plane of the transversalis fascia, or quadratus lumborum block is carried out. As described by the authors, this is a purely sensory block and so causes no muscle weakness or increase in the risk of falls. Following surgery, they injected 4-5 mg of morphine into the capsule, as well as 10 cc of 0.25% bupivacaine with epinephrine in the portals. In the postoperative period, the patients received 1-2 doses of 0.5 mg of intravenous (i.v.) morphine and 1-2 tablets of 5 mg of oxycodone via the oral route (p.o.). This form of multimodal analgesia reduced patient stay in the postsurgery recovery room as well as the number of readmissions due to poor pain control, compared with the group that only underwent nerve block(3).
In this same line, Fernicola et al. propose preoperative pericapsular nerve block to achieve good pain control without the risks of the other described block techniques(32).
Local infiltration analgesia (LIA) has demonstrated its efficacy in other orthopaedic surgeries and proves effective in arthroscopy of the hip, with a lesser cost compared with nerve blocks(33). Intraoperative infiltration of the portals used during arthroscopy, pericapsular infiltration and periacetabular infiltration, used isolatedly or in combination, appear to offer adequate postoperative analgesia without the risks described for some nerve block procedures(34,35,36,37). Garner and Sardesai performed local infiltration of the portals down to the joint plane, administering 40 ml of 0.25% levobupivacaine, with better results than following fascia iliaca block(1,38). The intraarticular infiltration of morphine and clonidine also appears to lessen postoperative pain and morphic drug use in the first hours after surgery, thereby reducing the side effects of such medication and affording improved patient satisfaction with the process(13). In this study, anti-inflammatory drugs were also administered preoperatively, in the same way as in other studies commented above. Another randomised prospective study comparing lumbar plexus block versus pericapsular infiltration documented similar pain control with fewer complications(39).
In our opinion, pericapsular infiltration and infiltration of the portals used during arthroscopy affords a level of postoperative analgesia similar to that obtained with peripheral nerve blocks, though with fewer complications, and so may be regarded as a first choice in this type of procedure.
Postoperative pain control
A number of drugs have been found to be useful for the management of postoperative pain in arthroscopy of the hip: NSAIDs, analgesics (non-opiate drugs such as paracetamol, and opiates) and gabapentin and its derivatives(9,40,41).
The use of NSAIDs, especially of COX-2 inhibitors and naproxen, in patients subjected to arthroscopy of the hip appears to offer a dual benefit, since it can help to control postoperative pain and to reduce the incidence of the heterotopic calcifications that sometimes appear after this type of surgery — though the dosage, duration and impact of such treatment upon the prognosis have not been clearly established(42,43,44).
The duration of postoperative analgesic treatment is highly variable. In the study published by García, over 50% of the surgeons prolonged the duration of treatment between one and two weeks. It has been reported that approximately 25% of the patients continue to use opiates for over three months after surgery. The most important risk factor for postoperative opiate use is the preoperative administration of such drugs. A negative influence is also exerted by the use of anxiolytics, the abuse of addictive substances, morbid obesity and low back pain. Prolonged opiate consumption is associated to an increased probability of severe side effects and complications. Such consumption therefore should be avoided if possible(45), particularly considering that significant reduction of the opiate dose in the postoperative period does not seem to be related to greater patient satisfaction in terms of the sensation of pain control(37,46).
The interesting study published by Nguyen et al.(47) divided the patients according to the type of postoperative pain, defining a group of fast starters (i.e., patients with a rapid start of recovery), presenting minimum discomfort and with a desire to become involved in new activities one week after surgery, versus a group of slow starters (i.e., patients with a slow start of recovery), characterised by severe pain and important limitations. A positive correlation was found between pain at one week (VAS score) and pain at two years, as well as better results on the functional scales after two years, among the fast starters.
Rehabilitation also contributes to postoperative pain control. Most of the protocols divide the rehabilitation of patients subjected to arthroscopy of the hip into four phases. In the first phase, the fundamental objective is protection of the hip and preservation of its flexibility and mobility. Emphasis is placed on manual therapy, isometric exercises (glutes, quadriceps, ischiotibial muscles, abductors and adductors), and combined exercises of the hip and trunk(48).
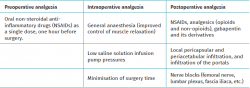
Recommendations (Table 1)
The main elements of the proposed multimodal approach are:
- Adequate preoperative analgesia. The current tendency is to administer NSAIDs as a single dose one hour before surgery.
- Adequate intraoperative analgesia, fundamentally based on the administration of drugs, pericapsular and periacetabular local infiltrations, as well as infiltrations of the portals used during surgery. Nerve blocks (femoral nerve, lumbar plexus, fascia iliaca...) are presently more controversial for two reasons. The first reason is the complex anatomy of the innervation of the hip, which makes it difficult to achieve complete hip analgesia by means of nerve blocks, and the second reason is the risk of complications, particularly motor block, which increases the risk of falls.
- Adequate postoperative analgesia, fundamentally pharmacological. The most widely used drugs are NSAIDs, followed by analgesics (opioids and non-opioids), and gabapentin and its derivatives.
Conclusions
A multimodal management of perioperative pain in arthroscopy of the hip is clearly the best approach to secure correct pain control; patient satisfaction with the surgical procedure; lowered opiate use, with fewer side effects of such drugs; a shorter stay in the postsurgery recovery room and in hospital; and fewer readmissions due to poor pain control. The combination of correct pre- and postoperative analgesia, a careful surgical technique, periarticular and periacetabular infiltrations and infiltrations of the portals used during surgery, as well as nerve blocks, are key elements for securing good perioperative pain control. The currently most controversial aspect of these techniques is referred to nerve blocks, since these may cause motor block, especially of the quadriceps muscle, with an increased risk of falls.
Información del artículo
Cita bibliográfica
Autores
Ana Castel Oñate
Unidad de Cadera. Hospital Universitario Príncipe de Asturias. Alcalá de Henares, Madrid
Grupo Ibérico de Preservación de Cadera (GIPCA)
Cirugía Ortopédica y Traumatología (COT). Hospital Universitario Príncipe de Asturias. Madrid
Oliver Marín Peña
Unidad de Cadera. Hospital Universitario Infanta Leonor. Madrid
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Infanta Leonor. Madrid
Ethical responsibilities
Conflicts of interest. The authors state that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Sardesai AM, Garner M, Khanduja V. Editorial Commentary: Pain After Hip Arthroscopy—Are We Truly Addressing the Problem? Arthroscopy. 2020 Apr 1;36(4):1045-7.
-
2García FL, Williams BT, Maheshwer B, et al. Pain management practice patterns after hip arthroscopy: an international survey. J Hip Preserv Surg. 2021 Apr 28;7(3):537-46.
-
3Kolaczko JG, Knapik DM, Kroneberger E, Chadha A, Salata MJ. A comprehensive three-phase opiate sparing multimodal pain protocol for hip arthroscopy: a retrospective review. J Hip Preserv Surg. 2021 Apr 28;7(3):547-53.
-
4Castel-Oñate A, Marín Peña O, García-Esteo FJ, et al. Estudio anatómico de la extravasación de líquido a la cavidad abdominal durante la artroscopia de cadera. Rev Esp Artrosc Cir Articul. 2020 Dec;27(4).
-
5Rosenblum A, Landy DC, Perrone MA, Whyte N, Kang R. The Presence of a Psychiatric Condition is Associated With Undergoing Hip Arthroscopy for Femoroacetabular Impingement: A Matched Case-Controlled Study. J Arthroplasty. 2019 Mar 1;34(3):446-9.
-
6Sochacki KR, Brown L, Cenkus K, Di Stasi S, Harris JD, Ellis TJ. Preoperative Depression Is Negatively Associated With Function and Predicts Poorer Outcomes After Hip Arthroscopy for Femoroacetabular Impingement. Arthroscopy. 2018 Aug 1;34(8):2368-74.
-
7Zacharias AJ, Lemaster NG, Hawk GS, et al. Psychological Healthcare Burden Lessens After Hip Arthroscopy for Those With Comorbid Depression or Anxiety. Arthrosc Sports Med Rehabil. 2021 Jun 17;3(4):e1171-e1175.
-
8Tan CO, Chong YM, Tran P, Weinberg L, Howard W. Surgical predictors of acute postoperative pain after hip arthroscopy. BMC Anesthesiol. 2015 Jul 2;15(1).
-
9LaPorte C, Rahl MD, Ayeni OR, Menge TJ. Postoperative Pain Management Strategies in Hip Arthroscopy. Curr Rev Musculoskelet Med. 2019 Dec 1;12(4):479-85.
-
10Shin JJ, McCrum CL, Mauro CS, Vyas D. Pain Management After Hip Arthroscopy: Systematic Review of Randomized Controlled Trials and Cohort Studies. Am J Sports Med. 2018 Nov;46(13):3288-98.
-
11Zhang Z, Zhu W, Zhu L, Du Y. Efficacy of celecoxib for pain management after arthroscopic surgery of hip: a prospective randomized placebo-controlled study. Eur J Orthop Surg Traumatol. 2014 Aug;24(6):919-23.
-
12Kahlenberg CA, Patel RM, Knesek M, Tjong VK, Sonn K, Terry MA. Efficacy of Celecoxib for Early Postoperative Pain Management in Hip Arthroscopy: A Prospective Randomized Placebo-Controlled Study. Arthroscopy. 2017 Jun;33(6):1180-5.
-
13Cogan CJ, Knesek M, Tjong VK, et al. Assessment of Intraoperative Intra-articular Morphine and Clonidine Injection in the Acute Postoperative Period After Hip Arthroscopy. Orthop J Sports Med. 2016 Feb 26;4(2):2325967116631335.
-
14Yap EN, Behrends M. Editorial Commentary: Neuraxial Anesthesia Improves Pain After Hip Arthroscopy but Risks Ambulatory Discharge Delay. Arthroscopy. 2021 Jan;37(1):147-8.
-
15Steinhaus ME, Rosneck J, Ahmad CS, Lynch TS. Outcomes After Peripheral Nerve Block in Hip Arthroscopy. Am J Orthop (Belle Mead NJ). 2018 Jun;47(6).
-
16Ward JP, Albert DB, Altman R, Goldstein RY, Cuff G, Youm T. Are femoral nerve blocks effective for early postoperative pain management after hip arthroscopy? Arthroscopy. 2012 Aug;28(8):1064-9.
-
17Birnbaum K, Prescher A, Heßler S, Heller KD. The sensory innervation of the hip joint - An anatomical study. Surg Radiol Anat. 1997;19(6):371-5.
-
18Kampa RJ, Prasthofer A, Lawrence-Watt DJ, Pattison RM. The internervous safe zone for incision of the capsule of the hip. A cadaver study. J Bone Joint Surg Br. 2007 Jul;89(7):971-6.
-
19Meheux CJ, Hirase T, Dong D, Clyburn TA, Harris JD. Healthy Hip Joints Have Different Macroscopic and Microscopic Capsular Nerve Architecture Compared With Hips With Osteoarthritis, Femoroacetabular Impingement Syndrome, and Developmental Dysplasia of the Hip: A Systematic Review. Arthrosc Sport Med Rehabil. 2021 Feb 1;3(1):e269-76.
-
20Dold AP, Murnaghan L, Xing J, Abdallah FW, Brull R, Whelan DB. Preoperative femoral nerve block in hip arthroscopic surgery: a retrospective review of 108 consecutive cases. Am J Sports Med. 2014 Jan;42(1):144-9.
-
21Childs S, Pyne S, Nandra K, Bakhsh W, Mustafa SA, Giordano BD. The Effect of Intra-articular Cocktail Versus Femoral Nerve Block for Patients Undergoing Hip Arthroscopy. Arthroscopy. 2017 Dec;33(12):2170-6.
-
22Xing JG, Abdallah FW, Brull R, et al. Preoperative Femoral Nerve Block for Hip Arthroscopy: A Randomized, Triple-Masked Controlled Trial. Am J Sports Med. 2015 Nov 1;43(11):2680-7.
-
23Childs S, Pyne S, Nandra K, Bakhsh W, Mustafa SA, Giordano BD. The Effect of Intra-articular Cocktail Versus Femoral Nerve Block for Patients Undergoing Hip Arthroscopy. Arthroscopy. 2017 Dec 1;33(12):2170-6.
-
24Oba M, Kobayashi N, Inaba Y, et al. Mechanical Strength of the Proximal Femur After Arthroscopic Osteochondroplasty for Femoroacetabular Impingement: Finite Element Analysis and 3-Dimensional Image Analysis. Arthroscopy. 2018 Aug 1;34(8):2377-86.
-
25Behrends M, Yap EN, Zhang AL, et al. Preoperative fascia iliaca block does not improve analgesia after arthroscopic hip surgery, but causes quadriceps muscles weakness: a randomized, double-blind trial. Anesthesiology. 2018;129(3):536-43.
-
26Ranawat A. Preoperative Femoral Nerve Block Did Not Reduce Oral Opioid Consumption at 24 Hours and Increased Risk of Noninjurious Falls After Hip Arthroscopy. J Bone Joint Surg Am. 2016 Aug 17;98(16):1407.
-
27Lee S, Hwang JM, Lee S, et al. Implementation of the Obturator Nerve Block into a Supra-Inguinal Fascia Iliaca Compartment Block Based Analgesia Protocol for Hip Arthroscopy: Retrospective Pre-Post Study. Medicina (Kaunas). 2020 Mar 27;56(4):150.
-
28Yadeau JT, Tedore T, Goytizolo EA, et al. Lumbar plexus blockade reduces pain after hip arthroscopy: a prospective randomized controlled trial. Anesth Analg. 2012 Oct;115(4):968-72.
-
29Wolff AB, Hogan GW, Capon JM, Napoli AM, Smith HJ, Gaspar PS. Pre-operative lumbar plexus block provides superior post-operative analgesia when compared with fascia iliaca block or general anesthesia alone in hip arthroscopy. J Hip Preserv Surg. 2016 Jul 13;3(4):hnw021.
-
30Zimmerer A, Schneider MM, Sobau C, Miehlke W, Eichler F, Wawer Matos J. The Erector Spinae Plane Block in the Setting of Hip Arthroscopy: A Prospective Randomized Controlled Clinical Trial. Arthroscopy. 2022 Jan;38(1):65-71.
-
31McCrum CL, Ben-David B, Shin JJ, Wright VJ. Quadratus lumborum block provides improved immediate postoperative analgesia and decreased opioid use compared with a multimodal pain regimen following hip arthroscopy. J Hip Preserv Surg. 2018 Oct 25;5(3):233-9.
-
32Fernicola, Jacob Tannehill I, Tucker CJ, Robert Volk W, Dickens JF. The Pericapsular Nerve Group Block for Perioperative Pain Management for Hip Arthroscopy. Arthrosc Tech. 2021 Jul 1;10(7):e1799-803.
-
33Philippon MJ, Devitt BM, Campbell KJ, et al. Anatomic variance of the iliopsoas tendon. Am J Sports Med. 2014;42(4):807-11.
-
34Baker JF, McGuire CM, Byrne DP, Hunter K, Eustace N, Mulhall KJ. Analgesic control after hip arthroscopy: a randomised, double-blinded trial comparing portal with intraarticular infiltration of bupivacaine. Hip Int. 2011 May-Jun;21(3):373-7.
-
35Shlaifer A, Sharfman ZT, Martin HD, et al. Preemptive Analgesia in Hip Arthroscopy: A Randomized Controlled Trial of Preemptive Periacetabular or Intra-articular Bupivacaine in Addition to Postoperative Intra-articular Bupivacaine. Arthroscopy. 2017 Jan 1;33(1):118-24.
-
36Kazum E, Rath E, Shlaifer A, et al. Preemptive analgesia in hip arthroscopy: intra-articular bupivacaine does not improve pain control after preoperative peri-acetabular blockade. Hip Int. 2020 Aug 31:1120700020950247.
-
37Kunze KN, Polce EM, Lilly DT, et al. Adjunct Analgesia Reduces Pain and Opioid Consumption After Hip Arthroscopy: A Systematic Review of Randomized Controlled Trials. Am J Sports Med. 2020 Dec 1;48(14):3638-51.
-
38Garner M, Alsheemeri Z, Sardesai A, Khanduja V. A Prospective Randomized Controlled Trial Comparing the Efficacy of Fascia Iliaca Compartment Block Versus Local Anesthetic Infiltration After Hip Arthroscopic Surgery. Arthroscopy. 2017 Jan 1;33(1):125-32.
-
39Scanaliato JP, Christensen D, Polmear MM, Salfiti C, Gaspar PS, Wolff AB. Prospective Single-Blinded Randomized Controlled Trial Comparing Pericapsular Injection Versus Lumbar Plexus Peripheral Nerve Block for Hip Arthroscopy. Am J Sports Med. 2020 Sep 1;48(11):2740-6.
-
40Krych AJ, Baran S, Kuzma SA, Smith HM, Johnson RL, Levy BA. Utility of multimodal analgesia with fascia iliaca blockade for acute pain management following hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2014 Apr;22(4):843-7.
-
41Shing EZ, Leas D, Michalek C, Wally MK, Hamid N. Study protocol: randomized controlled trial of opioid-free vs. traditional perioperative analgesia in elective orthopedic surgery. BMC Musculoskelet Disord. 2021 Jan 23;22(1):104.
-
42Dow T, King JP, Wong IH. The Reduction of Heterotopic Ossification Incidence After Hip Arthroscopy in Patients Treated With Selective Cyclooxygenase 2 Inhibitor (Celecoxib). Arthroscopy. 2020 Feb;36(2):453-61.
-
43Rath E, Warschawski Y, Maman E, et al. Selective COX-2 Inhibitors Significantly Reduce the Occurrence of Heterotopic Ossification after Hip Arthroscopic Surgery. Am J Sports Med. 2016 Mar 1;44(3):677-81.
-
44Yeung M, Jamshidi S, Horner N, Simunovic N, Karlsson J, Ayeni OR. Efficacy of Nonsteroidal Anti-inflammatory Drug Prophylaxis for Heterotrophic Ossification in Hip Arthroscopy: A Systematic Review. Arthroscopy. 2016 Mar 1;32(3):519-25.
-
45Anciano Granadillo V, Cancienne JM, Gwathmey FW, Werner BC. Perioperative Opioid Analgesics and Hip Arthroscopy: Trends, Risk Factors for Prolonged Use, and Complications. Arthroscopy. 2018 Aug;34(8):2359-67.
-
46Bloom DA, Manjunath AK, Wang C, et al. Institutional Reductions in Opioid Prescribing Following Hip Arthroscopy Do Not Change Patient Satisfaction Scores. Arthrosc Sport Med Rehabil. 2021 Apr 1;3(2):e463-9.
-
47Nguyen TQ, Friedman JM, Flores SE, Zhang AL. Fast Starters and Slow Starters After Hip Arthroscopy for Femoroacetabular Impingement: Correlation of Early Postoperative Pain and 2-Year Outcomes. Am J Sports Med. 2020 Oct 1;48(12):2903-9.
-
48Bistolfi A, Guidotti C, Aprato A, et al. Rehabilitation Protocol After Hip Arthroscopy: A 2015-2020 Systematic Review. Am J Phys Med Rehabil. 2021 Oct 1;100(10):958-65.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- The importance of pain control
- Learning from pain to make the patient feel better
- Perioperative pain management in arthroscopic surgery of the shoulder
- Perioperative pain management in arthroscopy of the elbow
- Perioperative analgesia in arthroscopic surgery of the wrist and hand
- Perioperative analgesia in arthroscopy of the hip
- Perioperative analgesia in arthroscopic surgery of the knee
- Perioperative pain management in arthroscopy of the ankle
- Postoperative neuropathic pain in traumatology
- Capsaicin 179 mg patch application technique
- Type 3 SLAP: bucket handle tear
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.