Role of arthroscopy in the treatment of ankle fractures
Papel de la artroscopia en el tratamiento de las fracturas de tobillo
Resumen:
Introducción: las fracturas de tobillo suelen presentar lesiones intraarticulares no visibles en la cirugía abierta. La artroscopia permite evaluarlas y tratarlas.
Métodos: se revisa el papel de la artroscopia en fracturas de tobillo, especialmente en la detección y el tratamiento de lesiones ocultas, y la asistencia a la reducción articular.
Resultados: la artroscopia permite eliminar cuerpos libres, desbridar hematomas y valorar la congruencia articular. Mejora la detección de inestabilidad sindesmal (hasta 87%) y reduce los defectos en la reducción del maléolo medial (22-32%). Se asocia con mejores resultados funcionales y menos complicaciones.
Conclusión: la artroscopia optimiza el tratamiento de fracturas de tobillo complejas y debería considerarse sobre todo en casos de fracturas inestables.
Abstract:
Introduction: Ankle fractures usually present intra-articular injuries that are not visible in open surgery. Arthroscopy makes it possible to assess and treat them.
Methods: The role of arthroscopy in ankle fractures is reviewed, especially in relation to the detection and treatment of occult injuries, and in assisting joint reduction.
Results: Arthroscopy makes it possible to eliminate loose bodies, debride hematomas and assess joint congruence. It improves the detection of syndesmotic instability (up to 87%) and reduces medial malleolus reduction defects (22-32%). The use of arthroscopy is associated with better functional outcomes and fewer complications.
Conclusion: Arthroscopy optimizes the treatment of complex ankle fractures and should be considered especially in cases of unstable fractures.
Introduction
In recent years, research on ankle fractures has led to a better understanding of such fractures, and ligamentous injury has gained importance(1). In addition, the increasingly systematic use of computed tomography (CT) for diagnosis has led to improved assessment of these lesions(2).
Although open reduction and internal fixation (ORIF) remains the standard treatment in most hospitals, open surgery does not allow the assessment and treatment of concomitant intra-articular injuries. The main advantage of ankle arthroscopy is its ability to visualize the joint cartilage and ligaments, as well as to identify lesions that are not evident on conventional radiographs or during ORIF(3,4).
For more than 20 years, the literature has indicated that there is a high prevalence of intra-articular injuries associated with ankle fractures, such as chondral injuries, loose bodies and damage to ligaments. These injuries, if not identified and treated, can lead to unsatisfactory clinical outcomes, including persistent pain and the early development of post-traumatic osteoarthritis (PTOA)(5,6).
Arthroscopy can assist in the reduction of fractures, joint debridement, the removal of loose bodies and the treatment of cartilage and ligament damage. The most recent literature suggests that arthroscopy-assisted reduction and internal fixation (AAORIF) may offer improved functional outcomes and lower visual analogue scale (VAS) scores compared to traditional ORIF(3,5).
Regarding specific indications for use in ankle fractures, arthroscopy is recommended in fracture patterns associated with a high probability of intra-articular injury, such as high-energy fractures, Weber type B (supination external rotation [SER] and pronation abduction [PABD])and C (pronation external rotation [PER]) fibular fractures, and fractures with a high probability of injury to the syndesmosis(6).
Surgical technique
The therapeutic strategy begins with understanding the mechanism of injury and fracture pattern, planning the approaches and preparing the material to be used.
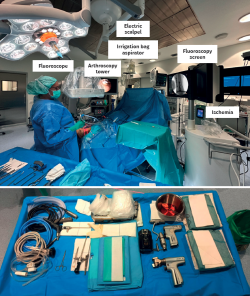
Placement in the operating room
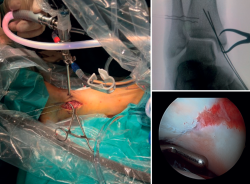
First, we adopt the posterior approach, if required by the fracture involved, and, after reducing the posterior malleolus, we place the patient in the supine position with a pad under the buttock. The ankle should be positioned at the edge of the operating table, which will allow free ankle flexion and extension, facilitating handling during arthroscopy. Ischemia and water aspiration and irrigation systems are placed on the same side as the fracture (but this may vary according to the technical peculiarities of each hospital). The arthroscopy tower and fluoroscope monitor are placed close to the patient's head and, on the contralateral side, we place the C-arm at the bottom to optimize visualization and arthroscopic and radiological access, allowing simultaneous use(7) (Figure 1 and Table 1).
Step-by-step surgical technique
Correct placement of the anteromedial (AM) and anterolateral (AL) portals is crucial in order to avoid damage to the saphenous and superficial peroneal nerves, respectively(7). Anterior ankle arthroscopy allows excellent access to zones 1, 2 and 3. Access to zones 4, 5 and 6 is more difficult. However, with plantar flexion and the instability generated by the fracture, osteochondral lesions (OCLs) in these Raikin quadrants can be visualized and treated(8,9).
1. Diagnostic and therapeutic arthroscopy
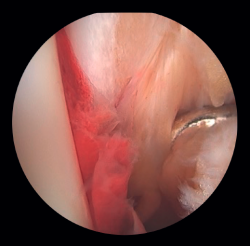
After osteosynthesis of the posterior malleolus, our next step is to perform diagnostic ankle arthroscopy to evaluate concomitant injuries such as OCLs or loose bodies, and to assess reduction of the posterior malleolus, and injuries to the external and internal ligament complex, and the syndesmosis. Although arthroscopy begins after the completion of osteosynthesis of the posterior malleolus, its use extends throughout the surgical procedure. In fractures without involvement of the posterior malleolus, arthroscopy is the first procedure to be performed prior to malleolar synthesis.
- Debridement of the joint and evacuation of the intra-articular hematoma: this could help eliminate proinflammatory markers that may play a role in the prevention of PTOA and reduce the occurrence of arthrofibrosis, which would have a positive effect on the prognosis of the fracture(10).
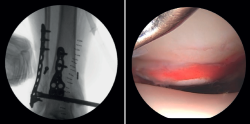
- Assessment of reduction of the posterior malleolus: arthroscopy can be used to verify reduction of the posterior malleolus(5) (Figure 2).
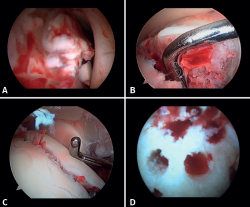
Lee has described a novel technique using a drill guide with ankle arthroscopy for the reduction of joint fragments in posterior malleolus fractures. In particular, this technique is beneficial for patients with trimalleolar fractures who have a depressed joint fragment, as it allows anatomical reduction and minimizes the need for extensive incisions(11). - Extraction of loose bodies. The presence of loose bodies within the joint is a common finding in ankle fractures. One-third of all arthroscopy patients had intra-articular loose bodies removed during surgery (24 out of 71cases)(12). Arthroscopy allows the precise removal of intra-articular loose bodies, which can cause pain, blockage or limitation of mobility, and damage to the joint cartilage(13).
- Management of chondral injuries. The literature reports the presence of chondral injuries in 34-91% of all ankle fractures. These lesions are frequently located in the talus and are most common in severe fractures, such as Weber C and PER fractures. Patients with cartilage lesions were 3.5 times more likely to develop radiographic osteoarthritis (Kannus arthritis score < 90) and 5 times more likely to have an unfavorable long-term clinical prognosis (American Orthopedic Foot and Ankle Society [AOFAS] score < 90)(14).
If possible, we reinsert unstable osteochondral fragments (Figure 3). In chondral lesions where it is not possible to reinsert the fragment, cartilage repair stimulation techniques can be used(5,13).
2. Open reduction and internal fixation of the lateral and/or medial malleolus
Arthroscopy assists ORIF in evaluating the congruence of the joint surface. It is especially useful for reduction of the medial malleolus. The malreduction rate in medial malleolus fractures is 22.2-32.6%(15,16). Initial arthroscopy allows us to determine whether tibial malleolus reduction can be performed in an open or closed manner. In cases with significant displacement, open synthesis is chosen, always maintaining arthroscopic control during the procedure to ensure precise reduction and avoid rotation of the distal fragment (Figure 4).
Patients at greatest risk of malreduction are those over 60 years of age, due to decreased bone quality and more complex fractures(17). Patients with open fractures and fracture dislocations have a 2.15 to 2.7 times higher risk, respectively, due to increased soft tissue damage and fracture complexity. Vertical fractures and with interposed soft tissues make it difficult to achieve anatomical reduction(15,16).
Xie (2025) and Liu (2020) compared AAORIF with ORIF(17,18). Less intraoperative blood loss, shorter hospital stays and faster healing times were observed in the first group(17,18). In addition, the postoperative inflammatory marker levels were lower, and the Olerud-Molander Ankle Score (OMAS) values at 6 months and one year were significantly higher than in the ORIF group(17,18).
3. Repair of ligament injuries
Following fracture synthesis, the ligament injuries are repaired.
- Assessment of the deltoid ligament. Tearing of the deltoid ligament can cause persistent medial instability after reduction of the fibula, associated with pain, dysfunction and the risk of PTOA if not adequately treated. Its repair in acute ankle fractures has been shown to improve reduction of the medial clear space (MCS) and the functional outcomes (AOFAS), and reduce postoperative complications. In SER type fractures, the assessment of medial stability is essential: while in SER II fractures the deep fascicle of the deltoid ligament is usually preserved, in SER IV fractures there is complete medial injury that compromises the tibiofibular mortise and requires surgical treatment(19).
The indications and criteria for deciding on deltoid ligament repair in patients with unstable ankle fractures include:
- Significant dislocation or widening of the MCS.
- Persistent medial instability despite peroneal fixation: if there is valgus instability or external rotation after anatomical reduction of the fibula, repair of the deltoid ligament is indicated.
- High-grade unstable fractures with syndesmotic instability.
In fractures with deltoid ligament damage, an increase in intra-articular injuries, such as osteochondral lesions, has been reported(19).
If the deltoid ligament injury involves only the anterior part, arthroscopic reinsertion can be made using resorbable implants. If deltoid ligament disinsertion is complete, open reinsertion is preferred, because of the difficulty of placing the implants in the posterior malleolus and the risk of neurovascular injury (Figure 5).
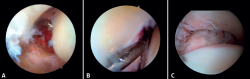
- Diagnosis of syndesmotic instability. Arthroscopy allows assessment of the integrity of the syndesmosis and the MCS on the radiograph and CT scan, especially in SER II and IV fractures. It has been shown that radiographic assessment is not always predictive of the syndesmotic lesion. In addition, arthroscopy ensures its anatomical reduction. Takao found that 87% (33/38) of the ankles with fractures had syndesmosis lesions detected by arthroscopy(20).
Arthroscopy allows both direct visualization and dynamic assessment of the syndesmosis(21,22).
- It makes it possible to differentiate between SER II fractures (where there should be no syndesmosis damage) and SER IV fractures, where the syndesmosis is affected and can be stabilized(5,23).
- Arthroscopy can avoid the false impression of a widened medial joint space on fluoroscopy due to congenital anomalies.
- Being able to visualize the malleolar incisura together with radioscopic control allows us to ensure correct positioning of the incisura fibularis, especially in patients with unstable injuries where there is a risk of malreduction due to shortening or rotation of the fibula(5,24).
- Arthroscopy can help avoid overcorrection of the syndesmosis, which is highly arthrogenic(5,24) (Figure 6).
Clinical and functional outcomes
Ankle fractures are very common injuries, with an average of 169/100,000 cases per year. The most commonly used method for treating unstable ankle fractures is ORIF. Even after anatomical reduction, some patients still experience persistent ankle pain and disability, possibly as a result of untreated intra-articular lesions(25).
Zhang performed a meta-analysis comparing ORIF with AAORIF in the treatment of unstable ankle fractures. The analysis yielded the following results: AAORIF showed better scores on the AOFAS and OMAS functional scales(26). On the AOFAS scale, AAORIF scored 91.0 versus 87.6 in the case of ORIF, while on the OMAS scale, AAORIF scored 90 versus 75 in the case of ORIF (p = 0.008). Patients subjected to AAORIF had lower postoperative pain VAS scores. The VAS scores were significantly lower on postoperative day 3 in the AAORIF group (1.96 ± 1.18) than in the RAFI group (2.83 ± 1.07). AAORIF allows the detection and treatment of intra-articular lesions, which may contribute to reduce the incidence of persistent pain and disability due to untreated injuries.
Other relevant findings reported by Zhang included the observation that AAORIF generally involves a longer surgery time. Specifically, the mean surgery time was 105.22 ± 27.13 minutes, versus 93.59 ± 22.79 minutes in the case of ORIF (p = 0.038). However, the complications rate was significantly lower with AAORIF (7.7% versus 27.5%; p = 0.006), as was the reoperations rate (1.5% versus 12.5%; p = 0.029), compared with ORIF. Finally, in this meta-analysis, no significant differences in early ankle PTOA rates were detected between AAORIF and ORIF, but better functional outcomes were recorded with AAORIF(27).
In a systematic review, Zhuang reported that AAORIF is more effective in the diagnosis and treatment of cartilage injuries, ligament damage and loose bodies. AAORIF detected more lesions of the syndesmosis than ORIF (80% versus 57.5%; p = 0.021). The incidence of these lesions was higher in the AAORIF group. This research group has also published better functional outcomes and scores on the VAS and OMAS scales compared to ORIF. HigherPatient-Reported Outcomes Measurement Information System (PROMIS) scores and satisfaction rates in Weber B ankle fractures treated with AAORIF were observed.
The reported complications during arthroscopic ankle procedures comprise superficial peroneal neuritis and damage to the neurovascular bundle. However, in comparison to ORIF, it has shown significantly lower rates of postoperative complications (7.7% versus 27.5%; p = 0.006) and revision surgeries (1.5% versus 12.5%; p = 0.029). The review also highlighted that occult intra-articular lesions are a cause of unsatisfactory outcomes in ankle fractures, and emphasized the diagnostic and prognostic usefulness of ankle arthroscopy in the prevention of PTOA(3,27).
Stabilization of the syndesmosis in ankle fractures is crucial to prevent chronic instability and PTOA. Trans-syndesmosis screw fixation has been the standard of care, but presents complications and biomechanical disadvantages.
Xie showed that stabilization of the syndesmosis with a dynamic fixation system offers equivalent functional results and fewer complications compared to screw fixation(28). AAORIF allows the evaluation of joint congruency after anatomical reduction of both the posterior and anterior syndesmosis. It also allows assessment of the overcorrection that can result from over-compression of the tibiofibular mortise, which has been shown to be highly arthrogenic(29). During reduction of the syndesmosis, help is provided by a palpation probe which we should be able to insert once the syndesmosis has been fixed.
AAORIF during ankle fracture fixation may improve the detection and treatment of syndesmosis instability. Liu, in a cadaveric model, found arthroscopy to be very sensitive in detecting sagittal and external rotation instability of the syndesmosis in the early stages of the injury, even with the application of low forces. More than twice as many patients with Weber type B or C fractures were seen to have arthroscopically detected instability of the syndesmosis (66%) compared to injuries detected by stress radiography (30.2%). The conclusion was that arthroscopy allows better determination of instability in multiple planes (sagittal and rotational) than fluoroscopy alone(5,21,30).
Hintermann reported that 79.2% of the patients with ankle fractures had damage to the joint cartilage, mostly located in the talus(30). The incidence was significantly increased in the case of Weber C fractures. In addition, 14.2% of the patients underwent arthroscopic removal of bone-cartilage fragments(30).
Cooper reviewed the long-term outcomes and return to sports activity in patients with ankle fractures, and described improved stability and quality of reduction with deltoid ligament repair(19). Such repair significantly reduces the incidence of malreduction and improves maintenance of the MCS, resulting in greater joint stability, better AOFAS and VAS scores, and lower revision surgery rates(19).
Deltoid ligament repair is associated with fewer revision surgeries compared to trans-syndesmosis fixation, mainly due to less material removal(5).
In terms of the return to sports activity, patients undergoing deltoid ligament repair have shown significant improvements in PROMIS, Foot and Ankle Ability Measure (FAAM) and numerical rating scale (NRS) scores, facilitating an earlier return to sports and a high level of activity.
In conclusion, deltoid ligament repair in unstable ankle fractures is indicated in cases of significant medial instability in high-grade unstable fractures(5,19).
Considerations and limitations
Despite the many advantages, there are some considerations and limitations to the use of arthroscopy in ankle fractures.
- Learning curve: the use of ankle arthroscopy and its application in fracture reduction has increased in recent years, particularly in the foot and ankle subspecialty. In this regard, it can be technically demanding and requires experience on the part of the surgeon(31).
- Limited evidence: although the evidence suggests benefits, there is a recognized need for further high quality randomized controlled studies to confirm these findings and establish clear indications for the use of arthroscopy in ankle fractures.
Conclusions
The use of arthroscopy in the treatment of ankle fractures offers significant advantages in terms of the diagnosis and treatment of concomitant intra-articular lesions that are often not diagnosed with the conventional techniques. It allows the direct assessment of joint congruency, the identification of occult lesions (cartilage, osteochondral and ligaments) and the possibility of repairing them, as well as direct monitoring of the fracture reduction achieved.
The current evidence suggests that AAORIF may afford superior functional outcomes and better pain control compared to ORIF alone. Although there are cost considerations and the need for technical expertise, the diagnostic and therapeutic advantages of arthroscopy make it a valuable tool that should be considered in order to optimize the management of ankle fractures and potentially improve the long-term patient outcomes. Further research is needed to fully define the role of arthroscopy in the management of these injuries, although we believe that the use of the arthroscope should be generalized in the treatment of ankle fractures.
Figuras
Figure 3. A: loose bodies; B: osteochondral lesion; C: reduction of the osteochondral lesion; D: medullary stimulation.
Figure 6. A: syndesmosis injury; B: control of reduction to avoid overcorrection; C: intraoperative control of correct reduction of the fibula at the incisura.
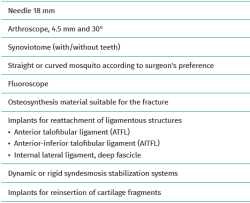
Tablas
Información del artículo
Cita bibliográfica
Autores
Deborah González García
Hospital Asepeyo Madrid
Unidad de Pie y Tobillo. Hospital Universitario de Guadalajara.
Complejo Hospitalario Ruber. Juan Bravo – Quirónsalud. Madrid
Elvira Iglesias Durán
Unidad de Miembro Inferior. Hospital Asepeyo Coslada. Madrid
Complejo Hospitalario Quirón Ruber Juan Bravo. Madrid
Universidad Europea. Madrid
Ethical responsibilities
Conflicts of interest. The authors declare that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work center referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Karanja AN, Ho-Huynh A, Walsh T, Platt SR. Ligamentous Injuries in Stable Ankle Fractures: An MRI-Based Study. Foot Ankle Orthop. 2025;10(1):24730114251328694.
-
2German J, Guillermo A, Rammelt S, et al. Quadrimalleolar Fractures of the Ankle: Think 360° —A Step-by-step Guide on Evaluation and Fixation. J Foot Ankle Surg (Asia Pacific). 2021;8(4):193-200.
-
3Zhuang C, Guo W, Chen W, et al. Arthroscopically assisted internal fixation for treatment of acute ankle fracture: A systematic review and meta-analysis of comparative studies. PLoS One. 2023;18(8):e0289554.
-
4Sherman TI. Editorial Commentary: Optimizing Surgical Management of Ankle Fractures: Is Arthroscopy the Answer? Arthroscopy. 2020;36(6):1722-4.
-
5Chan KB, Lui TH. Role of Ankle Arthroscopy in Management of Acute Ankle Fracture. Arthroscopy. 2016;32(11):2373-80.
-
6Da Cunha RJ, Karnovsky SC, Schairer W, Drakos MC. Ankle Arthroscopy for Diagnosis of Full-thickness Talar Cartilage Lesions in the Setting of Acute Ankle Fractures. Arthroscopy. 2018;34(6):1950-7.
-
7Connelly J, Ferkel RD. Ankle Arthroscopy: Correct Portals and Noninvasive Distraction. Arthroscopy. 2021;37(4):1066-7.
-
8Raikin SM, Elias I, Zoga AC, et al. Osteochondral Lesions of the Talus: Localization and Morphologic Data from 424 Patients Using a Novel Anatomical Grid Scheme. Foot Ankle Int. 2007;28(2):154-61.
-
9Phisitkul P, Akoh CC, Rungprai C, et al. Optimizing Arthroscopy for Osteochondral Lesions of the Talus: The Effect of Ankle Positions and Distraction During Anterior and Posterior Arthroscopy in a Cadaveric Model. Arthroscopy. 2017;33(12):2238-45.
-
10Sherman TI. Editorial Commentary: Optimizing Surgical Management of Ankle Fractures. Arthroscopy. 2020;36(6):1722-24.
-
11Lee HJ, Kim SJ, Park YU, et al. Use of an aiming drill guide and ankle arthroscopy for reduction of depressed articular surface in posterior malleolar fractures. J Orthop Surg (Hong Kong). 2021;29(3):23094990211055867.
-
12Smith KS, Drexelius K, Challa S, et al. Outcomes Following Ankle Fracture Fixation With or Without Ankle Arthroscopy. Foot Ankle Orthop. 2020;5(1):2473011420904046.
-
13Ono A, Nishikawa S, Nagao A, et al. Arthroscopically assisted treatment of ankle fractures: arthroscopic findings and surgical outcomes. Arthroscopy. 2004;20(6):627-31.
-
14Darwich A, Adam J, Dally FJ, et al. Incidence of concomitant chondral/osteochondral lesions in acute ankle fractures and their effect on clinical outcome: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2021;141(1):63-74. Erratum in: Arch Orthop Trauma Surg. 2021;141(8):1437-8.
-
15Baumfeld T, Burgos V, Souza V, et al. Ankle fractures malreduction rate and its causes in two Brazilian tertiary training hospitals. Injury. 2023;54 Suppl 6:110811.
-
16Hu J, Zhang C, Zhu K, et al. Adverse Radiographic Outcomes Following Operative Treatment of Medial Malleolar Fractures. Foot Ankle Int. 2018;39(11):1301-11.
-
17Liu C, You JX, Yang J, et al. Arthroscopy-Assisted Reduction in the Management of Isolated Medial Malleolar Fracture. Arthroscopy. 2020;36(6):1714-21.
-
18Xie X, Ji D, Chen F, et al. Arthroscopic Versus Open Fixation for Medial Malleolus Fractures Improves Trauma Response and Bone Healing. Sci Rep. 2025;15(1):15050.
-
19Cooper MT. The Role of Deltoid Repair and Arthroscopy in Ankle Fractures. Clin Sports Med. 2020;39(4):733-43.
-
20Lui TH, Ip K, Chow HT. Comparison of radiologic and arthroscopic diagnoses of distal tibiofibular syndesmosis disruption in acute ankle fracture. Arthroscopy. 2005;21(11):1370.
-
21Takao M, Ochi M, Naito K, et al. Arthroscopic diagnosis of tibiofibular syndesmosis disruption. Arthroscopy. 2001;17(8):836-43.
-
22Huang Q, Cao Y, Yang C, et al. Diagnosis of tibiofibular syndesmosis instability in Weber type B malleolar fractures. J Int Med Res. 2020;48(7):300060520939752.
-
23Chiang CC, Tzeng YH, Jeff Lin CF, et al. Arthroscopic Reduction and Minimally Invasive Surgery in Supination-External Rotation Ankle Fractures: A Comparative Study With Open Reduction. Arthroscopy. 2019;35(9):2671-83.
-
24Lui TH, Ip K, Chow HT. Comparison of radiologic and arthroscopic diagnoses of distal tibiofibular syndesmosis disruption in acute ankle fracture. Arthroscopy. 2005;21(11):1370.
-
25Van Dijk CN, Reilingh ML, Zengerink M, et al. Osteochondral defects in the ankle: why painful? Knee Surg Sports Traumatol Arthrosc. 2010;18:570-80.
-
26Leeb BF, Andel I, Sautner J, et al. The differentiation of inflammatory and non-inflammatory joint diseases with a diagnostic algorithm for clinicians. Rheumatology (Oxford). 2004;43(2):150-7.
-
27Zhang G, Chen N, Ji L, et al. Arthroscopically assisted versus open reduction internal fixation for ankle fractures: a systematic review and meta-analysis. J Orthop Surg Res. 2023;18(1):118.
-
28Xie L, Xie H, Wang J, et al. Comparision of suture button fixation and syndesmotic screw fixation in the treatment of distal tibiofibular syndesmotic injury: A systematic review and metaanalysis. Int Surg. 2028;60:120-31.
-
29Lui TH, Ip K, Chow HT. Arthroscopic Evaluation of Syndesmotic Instability in a Cadaveric Model. Foot Ankle Int. 2015;36(11):1362-8.
-
30Hintermann B, Regazzoni P, Lampert C, et al. Arthroscopic Findings in Acute Fractures of the Ankle. The Journal of Bone and Joint Surgery. British Volume. 2000;82(3):345-51.
-
31Shamrock AG, Khazi ZM, Carender CN, et al. Utilization of Arthroscopy During Ankle Fracture Fixation Among Early Career Surgeons: An Evaluation of the American Board of Orthopaedic Surgery Part II Oral Examination Database. Iowa Orthop J. 2022;42(1):103-8.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Anterior ankle arthroscopy at its best
- Foot and ankle arthroscopy, a consolidated and expanding reality
- The history and current concepts of ankle arthroscopy
- Current status of anterior ankle impingement
- Arthroscopic treatment of chronic lateral ankle instability
- Managing osteochondral lesions of the talus with anterior ankle arthroscopy
- Role of arthroscopy in syndesmosis injuries
- Role of arthroscopy in the treatment of ankle fractures
- Anterior arthroscopic ankle arthrodesis
- The use of needle arthroscopy in the ankle
- The letter pi on the ankle
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.