Role of arthroscopy in syndesmosis injuries
Papel de la artroscopia en las lesiones de la sindesmosis
Resumen:
Objetivo: analizar el papel diagnóstico y terapéutico de la artroscopia en las lesiones de la sindesmosis y del complejo ligamentoso medial del tobillo.
Métodos: se realizó una revisión centrada en la anatomía, la biomecánica, el diagnóstico clínico y por imagen, y el abordaje artroscópico tanto de lesiones agudas como crónicas de la sindesmosis y del ligamento deltoideo. Se describen las técnicas quirúrgicas más frecuentes, sus indicaciones y la evidencia disponible en la literatura.
Resultados: la artroscopia de tobillo permite una evaluación directa de la sindesmosis y del complejo medial. El uso de artroscopia permite reducir la tasa de malreducción de la sindesmosis (hasta 16-52% con técnicas abiertas) y detectar lesiones intraarticulares asociadas en hasta el 50% de los casos. La reparación artroscópica del ligamento deltoideo permite la reinserción de las fibras profundas del ligamento tibiotalar de forma efectiva.
Conclusiones: la artroscopia ofrece ventajas diagnósticas y terapéuticas en las lesiones de la sindesmosis y del complejo medial, mejorando la precisión de la reducción y permitiendo un tratamiento mínimamente invasivo de lesiones asociadas.
Nivel de evidencia: nivel IV.
Abstract:
Objective: to analyse the diagnostic and therapeutic role of arthroscopy in syndesmotic and medial ligament complex injuries of the ankle.
Methods: a focused review was conducted addressing the anatomy, biomechanics, clinical and imaging diagnosis, and the arthroscopic management of both acute and chronic injuries of the syndesmosis and the deltoid ligament. The most commonly used surgical techniques, their indications, and the available evidence from the literature are described.
Results: ankle arthroscopy allows direct assessment of the syndesmosis and medial ligament complex. Its use reduces the rate of syndesmotic malreduction (16-52% with open techniques) and identifies associated intra-articular injuries in up to 50% of cases. Arthroscopic deltoid ligament repair enables effective reinsertion of the deep tibiotalar fibres.
Conclusions: arthroscopy provides diagnostic and therapeutic advantages in syndesmotic and medial complex injuries, improving reduction accuracy and allowing minimally invasive treatment of associated lesions.
Level of evidence: level IV.
Introduction
Injuries affecting the syndesmosis (the fibrous attachment between the tibia and fibula at the ankle) and the medial ligament complex (deltoid ligament) are of great importance in the overall stability of the tibiotalar joint(1). Because they are not as common as lateral sprains, they sometimes go unnoticed or are underdiagnosed, leading to chronic instability, persistent pain and, in the long term, early osteoarthritis(2).
The syndesmosis is composed of the anterior tibiofibular ligament, the posterior tibiofibular ligament, the interosseous ligament and the transverse ligament(3). Each of these elements is involved in containing the joint against axial and rotational loads. The medial complex, consisting of the superficial and deep deltoid ligament, ensures stability in the frontal plane and prevents excessive eversion(4).
The arthroscopic approach has established itself as a highly valuable diagnostic and therapeutic tool. On the one hand, ankle arthroscopy offers a more accurate diagnosis by allowing direct observation of ligament integrity, the presence of chronic synovitis, and associated osteochondral lesions(5). On the other hand, it facilitates minimally invasive surgical procedures, with less morbidity than open approaches, and with potentially shorter recovery times.
This chapter reviews the anatomical and biomechanical aspects of the syndesmosis and medial ligament complex, the relevance of their injuries, the use of arthroscopy in their diagnosis and treatment, and the surgical techniques most endorsed by the current literature.
Anatomy and biomechanics
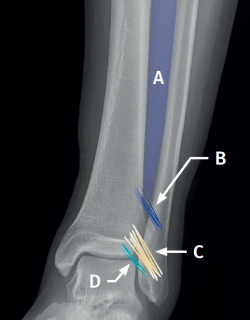
Syndesmosis (Figure 1)
The syndesmosis is a fibrous ring that joins the tibia and fibula distally(1). Its main function is to maintain the congruence of the tibiofibular mortise and to allow physiological micromovements of separation and rotation of the fibula with respect to the tibia(6).
It is composed of:
- The anterior tibiofibular ligament (ATFL). Considered to be the first to be injured by external rotation or forced dorsiflexion forces. It extends obliquely from the anterior tubercle of the distal tibia, approximately 5 mm above the joint surface, to the anterior tubercle of the distal fibula, running proximal-medial to distal-lateral and crossing the anterolateral corner of the talus(7).
- The ATFL has a constant distal fascicle (ATFL-DF) that contacts the anterolateral corner of the talus when the ankle is in neutral position. The distal fibers of the ATFL-DF continue with the upper bundle of the anterior talofibular ligament(8).
- The posterior tibiofibular ligament (PTFL), which is stronger than the anterior ligament. It extends from the posterior tibial malleolus to the posterior tubercle of the fibula and runs proximal-medial to distal-lateral. It forms an angle of 20º to40° with the horizontal plane.
- The interosseous ligament (IL), a distal thickening of the interosseous membrane that acts as a "spring" or dynamic stabilizer.
- The transverse ligament, located in the most posterior part, and considered by some authors as the distal portion of the PTFL.
Arthroscopic anatomy of the syndesmosis
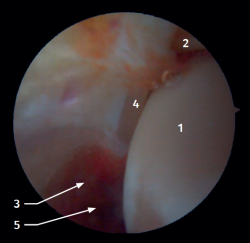
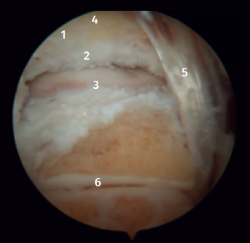
Anterior arthroscopic view
Twenty percent of the ATFL is intra-articular(7). On adopting an anteromedial access of the ankle, directing the arthroscope laterally, we can see the distal fibers of the ATFL with their oblique distribution and their continuation with the anterior talofibular ligament (Figure 2). If we move into the tibiotalar joint, we see the distal tibiofibular joint with the syndesmotic recess occupied by synovial tissue (Figure 3).
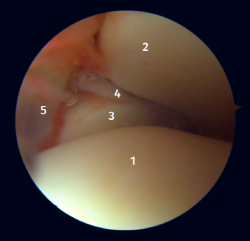
Posterior arthroscopic view
From the posterolateral approach we identify the lateral (fibular) malleolus and, from here, we visualize the intra-articular fibers of the PTFL, which run obliquely and insert into the distal portion of the tibia. We also see the distal thickening of the PTFL (transverse ligament) in continuity with the posterior lip of the distal tibia (Figure 4).
Medial complex
The medial ankle complex, also known as the medial collateral ligament, is a broad, tough fibrous structure located on the medial (internal) side of the joint. Anatomically, this ligament exhibits a fan- or delta-shaped configuration and is made up of two main layers: superficial and deep(9).
The superficial layer is composed of several bands which are divided into:
- The tibionavicular ligament, which arises from the anterior aspect of the medial malleolus and runs towards the navicular bone.
- The tibiocalcaneal ligament, with insertion in the sustentaculum tali.
- The tibiospring ligament, which reinforces the junction with the spring ligament (calcaneonavicular ligament) and stabilizes the medial aspect of the ankle.
- The superficial tibiotalar band, which is directed towards the medial aspect of the talus, reinforcing containment.
The deep layer in turn is composed of:
- The deep anterior tibiotalar ligament, which arises from the anterior aspect of the medial malleolus and inserts on the medial surface of the talus.
- The more robust deep posterior tibiotalar ligament, which runs to the posterior portion of the talus and contributes to anteroposterior stability.
Both layers are in close relationship with the tibialis posterior tendon sheath, which enhances mechanical effectiveness in containing the joint, counteracting excessive hindfoot eversion and avoiding lateral translation of the talus.
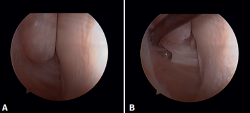
Arthroscopic anatomy of the medial complex
Arthroscopy allows us to see the deep fibers of the deltoid ligament, corresponding to the intra-articular portion of the ligament. Medial and proximal to the tip of the malleolus we have the insertion of the deep layer of the deltoid ligament. If there is no injury, we will see the anterior portion of the deep tibiotalar fibers. When injury is present, we can visualize the intermediate and posterior portion. The superficial bands, due to their more external location, are not visible by arthroscopy, unless there is no lesion of the deep bands (Figure 5).
Biomechanics
The deltoid ligament and syndesmosis act together to limit movement of the fibula relative to the tibia, mainly blocking external rotation of the talus. This effect is achieved by keeping the mortise reduced, avoiding lateral displacement of the talus towards the lateral malleolus.
In practice, the deltoid ligament and the syndesmosis should be considered as a single unit performing the same biomechanical function. Therefore, when a lesion of one of these structures is detected, it is essential to examine the other, since the lesions are very often combined(10).
Epidemiology and clinical relevance
Although isolated lesions of the syndesmosis or medial complex represent a smaller percentage than lateral lesions, their relevance has been increasing. Epidemiological studies in contact sports athletes (football, rugby, basketball) describe that 10-20% of all ankle sprains may involve some degree of syndesmotic injury(11). These injuries can be associated with significant morbidity and a delayed return to sports compared to an isolated lateral ankle sprain(12).
The posterior syndesmosis plays the most important role, providing 40-45% of the resistance to diastasis, while the ATFL contributes about 35%. Injuries to two of the components of the syndesmosis result in a loss of more than 50% of diastasis resistance, which can lead to instability(13).
Isolated deltoid ligament injuries account for approximately 3-4% of all ankle ligament injuries(14). Isolated injury to the deltoid ligament usually affects the superficial portion, is rotationally stable, and has a good prognosis. In contrast, in deltoid injuries associated with injury to the syndesmosis, rupture is complete in both layers (deep and superficial)(15).
Diagnosis
A correct diagnosis is essential, as many injuries are underdiagnosed and will lead to sequelae. The most important point is to be able to differentiate between stable injuries, which can be treated on a conservative basis, and unstable injuries.
Clinical assessment
Patients often present with anterior ankle pain, a feeling of instability and limited dorsiflexion. Specific clinical tests include:
- Squeeze test. This test is more specific of syndesmosis injuries. With the patient seated, the examiner presses with both hands on the tibia and fibula, starting just above the ankle. If the pressure causes pain in the distal syndesmosis, injury to its ligaments is suspected.
- The dorsiflexion maneuver. This is performed to push the wider anterior portion of the talar trochlea into the ankle mortise, causing separation of the distal fibula and tibia and pain in the distal tibiofibular syndesmosis.
- Deltoid stress maneuver. This is performed with the patient seated on the stretcher and the feet dangling. First, valgus pressure to the heel is applied, comparing the response with that of the sound ankle. The anterior drawer maneuver is then performed and the result is also contrasted with that of the contralateral side. The external lateral ligament is also involved in anterior drawer stability.
- Selective palpation of the syndesmosis and deltoid ligament. Pain on deltoid palpation is associated with injury, with Hinterman reporting a correlation of 100%(16). In contrast, for the diagnosis of syndesmotic injuries, the figure drops to 56%(17).
Imaging tests
- Plain radiography: in anteroposterior, mortise and lateral views, signs of diastasis of the syndesmosis are observed if the tibiofibular space exceeds 5-6 mm or in the absence of tibiofibular overlap below 6 mm. In many cases the degree of diastasis is not clearly visible in subacute or chronic stages.
- Computed tomography (CT): this technique helps to assess the position of the fibula in the tibial incisura and to detect small anterior or posterior subluxations.
- CT in weight bearing: most useful in cases of suspected subtle lesions of the syndesmosis and deltoid ligament. Three-dimensional (3D) volume measurements by CT in weight bearing reach a sensitivity of 95.8% and a specificity of 83.3% in detecting unstable lesions of the syndesmosis(18).
- Magnetic resonance imaging (MRI): this is the most sensitive test, reaching a sensitivity of 100% and a specificity of 93% in ATFL lesions(19). However, unlike the weight bearing CT scan, MRI has the limitation that it is not always possible to determine with certainty whether the lesion is accompanied by obvious instability of the syndesmosis.
Ankle arthroscopy
Ankle arthroscopy is the gold standard technique for ligament injuries of the ankle. It provides the diagnosis in doubtful cases and is able to define the real extent of the lesion. In addition, it allows the assessment of intraoperative stability.
Arthroscopic evaluation of the syndesmosis
From the anteromedial portal we can directly visualize the distal fibers of the ATFL. Disinsertion of these fibers does not always result in instability of the syndesmosis, but it does require us to check it. In our experience, we prefer assessment of the coronal plane of the syndesmosis. We introduce the arthroscope into the tibiotalar joint directing the camera cranially. In this way we have a direct view of the distal tibiofibular joint. We then assess stability by attempting to insert the palpation probe into the joint. If it is possible to do so, we classify the syndesmosis injury as unstable (Figure 6A).
Arthroscopic evaluation of the deltoid ligament
There are multiple methods for assessing instability of the medial complex; using the anterior ankle portals it is possible to assess the stability of the deltoid ligament in its main plane of action, corresponding to the coronal plane. Chun et al.(20) described instability when it is possible to introduce an arthroscopic palpation probe into the medial tibiotalar space (Figure 6B). Vega et al.(21) reported that, in the majority of injuries, the most anterior portion of the deltoid ligament is detached from the medial malleolus, while its proximal insertions remain intact. In this situation, the arthroscopic palpation probe can be inserted between the medial wall of the internal malleolus and the deep fibers of the deltoid ligament.
Arthroscopic treatment of the syndesmosis and medial complex
Arthroscopic treatment of syndesmosis injuries
There is consensus that a stable injury can be treated on a conservative basis, which includes a period without weight bearing, followed by protected partial weight bearing (with a walking boot) and a rehabilitation protocol(22).
An unstable injury requires surgery to avoid long-term sequelae(23). Ankle arthroscopy remains central to diagnosis and treatment, and it is vital to decide which injuries need to be repaired. Direct visualization of the distal tibiofibular joint is the most accurate way to assess the degree of injury. The association of a deltoid ligament lesion is strongly predictive of an unstable injury.
In addition, up to half of all injuries of the syndesmosis may have concomitant intra-articular disorders (osteochondral lesions or loose bodies)(24), which reinforces the role of arthroscopy for both diagnosis and simultaneous treatment.
It should be noted that injury to the syndesmosis causes disruption of the tibiofibular joint in the coronal and/or sagittal plane. The incidence of joint malreduction when compression clamp reduction is used is 16-52%(25,26). Given these percentages, the use of arthroscopy as a method for controlling reduction is growing in importance.
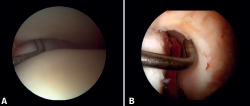
Surgical technique: arthroscopic treatment of acute syndesmosis injuries
The technique should be performed using the conventional anteromedial and anterolateral portals. The anteromedial portal is used for visualization, while the anterolateral portal serves as the working portal. Once the tibiofibular space is visualized, the inflamed synovial component is resected with an arthroscopic shaver to facilitate reduction (Figure 7A). Then, under direct vision, we restore the tibiofibular space, carefully taking into account possible malrotation of the fibula, especially in Maisonneuve type fractures. For fibular reduction we use a Verbrugge clamp, which allows us to correct the rotation. In our experience, once the space has been cleaned and if the position is correct, it is infrequent to have to use a compression clamp between the tibia and fibula.
Once the desired reduction has been achieved, we visually check the position and temporarily fix it using a Kirschner pin.
For definitive fixation, the surgical options range between rigid fixation with screws and dynamic fixation. Screws have been the standard procedure for decades, but involve complications, such as loosening or rupture. Furthermore, some surgeons advocate their removal, with the inherent risk of recurrence of instability(27). Dynamic fixation was designed to overcome some of these problems by allowing a degree of physiological movement of the syndesmosis, facilitating early weight bearing, reducing the risk of rupture, and eliminating the need to remove the implant (Figure 7B).
Grassi et al., in a meta-analysis involving over 300 patients, demonstrated an overall decrease in the relative risk of complications (RR = 0.55, p = 0.003) with dynamic systems(28). Raeder et al., in a randomized trial of 97 patients contrasting screw fixation versus a dynamic system, reported a lower incidence of osteoarthritis with suture buttons of 65% versus 35% (p = 0.009) at 5 years(29). Suture button constructions afford a degree of micro-mobility, mimicking physiological mobility, which can promote ligament healing. Likewise, flexible implants are better able to tolerate an imperfect reduction, as a possible complication, even if arthroscopic control of the joint is performed.
Surgical technique: arthroscopic treatment of chronic syndesmosis injuries
Chronic lesions of the syndesmosis are usually underdiagnosed and remain unidentified in a significant percentage of cases. Ankle arthroscopy is an essential tool, with clearly proven efficacy, for the diagnosis and assessment of this type of injury.
The principles referred to fixation are the same, but a more solid option should be chosen, with double screws, double dynamic fixation, or mixed techniques(30,31). Some authors describe techniques involving syndesmosis plasty procedures with autografts (hamstring or peroneus).
Currently, there is insufficient scientific evidence in favor of one surgical technique over another in patients with chronic injuries of the syndesmosis(32,33), and there is a lack of clinical trials to decide which treatment is superior.
The technique used in our practice is the arthroscopic technique without reinforcement plasty. Meticulous arthroscopic debridement of the lower tibiofibular joint is essential to allow complete reduction of the joint. Regarding the type of fixation, we consider that chronic injuries have a higher degree of instability that requires greater fixation, with our preference being the use of a double dynamic system.
Injuries of the medial complex
The deltoid ligament is essential for medial stability of the ankle, as it limits valgus, excessive rotation and anterior translation of the talus. There are usually three main reasons for damage to this ligament: an isolated injury caused by valgus and forced external rotation, associated with chronic lateral instability or in relation to posterior tibial deficiency, producing medial instability as a result(34). Clinically, it presents as anteromedial pain and a feeling of laxity.
The aim of deltoid ligament repair is to reduce external rotation, eversion and anterior translation, since increasing these movements can lead to early osteoarthritis of the ankle(35). In lateral instability in patients with hyperlaxity or severe injury, repair of the anterior portion of the deltoid ligament provides greater fixation to limit anterior translation of the talus(21).
Arthroscopic treatment of medial complex injuries
The deltoid ligament of the ankle can be repaired by open or arthroscopic surgery. While there is ample evidence supporting the safety and efficacy of the open technique(36), comparative studies have emerged in recent years showing similar clinical and radiological results with arthroscopic repair(37). The latter has the advantage of being less aggressive on the soft tissues, which is particularly relevant in trauma patients. It also allows us to simultaneously address other intra-articular lesions.
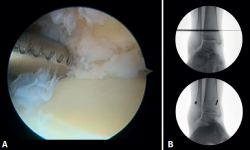
Surgical technique: arthroscopic treatment of acute medial complex injuries
In terms of surgical technique, the working portals are established in the same way as in conventional ankle arthroscopy: one anteromedial portal and one anterolateral portal. We always start with diagnostic arthroscopy to confirm the injury to the deltoid ligament. A probe can be used to verify the laxity of the fibers, and a test can be performed by inserting the probe through the medial groove: the lesion is confirmed if the instrument passes through. For repair, the viewing portal will be the anterolateral portal, thus allowing us to work more directly through the anteromedial portal. The anterior fibers of the superficial tibiotalar and intermediate fibers of the deep portion of the deltoid ligament are the ones that can be repaired with the arthroscopic technique(38). Once the ligament has been identified and dissected, a suture is passed between the fibers using a suture passer. The medial malleolus anchorage zone is prepared with a shaver or a small burr. With the ankle in neutral position, the anchor is inserted while maintaining the tension of the sutures. The intersection of the line parallel to the tibiotalar joint and a perpendicular line marked from the tip of the malleolus and along the lateral border of the malleolus can be used as an anatomical reference for placement(21). After reduction, we again test the fibers for tension and passage of the probe through the medial groove, to confirm adequate repair (Figure 8).
Arthroscopic treatment of chronic medial complex injuries
Ankle arthroscopy is also useful in the treatment of chronic deltoid ligament injuries. Initially, arthroscopy helps to assess the severity of the injury, as well as in treating associated disorders such as osteophytes or cartilage lesions. In severe cases where there is already axial involvement leading to flat foot, additional repair procedures such as correction via calcaneal osteotomy should be considered.
The quality of the ligament with a chronic injury sometimes does not allow repair; in such cases we consider reconstruction performing an autologous graft plasty, e.g., using a gracilis graft or allograft. Loozen et al. recommended reconstruction of both the posterior deep fibers and the anterior tibiotalar fibers, and also added repair to the springligament(36). The results obtained with reconstruction are optimal. However, as Savage-Elliot et al.comment in their article, the repair of a reconstruction is not comparable, since in the latter case there are usually many more associated lesions due to the chronicity of the disorder, and what is intended is mainly to salvage the joint(39).
Conclusions
Ankle arthroscopy is a valuable diagnostic and therapeutic tool for ankle ligament injuries. In the case of the syndesmosis, direct visualization allows accurate assessment of stability, reduces the high incidence of malreduction seen with open techniques, and facilitates the simultaneous treatment of associated intra-articular lesions. In the case of the deltoid ligament, arthroscopy makes it possible to accurately identify the tear, repair the deep fibers and address concomitant injuries, with the advantage of less aggression to the soft tissues - this being particularly relevant in trauma patients.
Figuras
Figure 1. Schematic representation of the anterior syndesmosis. A: interosseous membrane; B: interosseous ligament; C: anterior tibiofibular ligament; D: distal fascicle of the anterior tibiofibular ligament.
Figure 2. Anterolateral arthroscopic view of the right ankle. 1: talar dome; 2: anterior aspect of the tibia; 3: fibula; 4: distal fibers of the anterior tibiofibular ligament; 5: anterior talofibular ligament.
Figure 3. Anterolateral arthroscopic view of a right ankle on entering the tibiotalar zone. 1: talar dome; 2: articular aspect of the tibia; 3: fibula; 4: distal tibiofibular joint; 5: distal fibers of the anterior tibiofibular ligament.
Figure 4. Posterior arthroscopic view of a right ankle in which a symptomatic Stieda process has been resected. 1: posterior tibiofibular ligament; 2: transverse ligament; 3: talar dome; 4: distal tibia; 5: posterior subtalar joint; 6: flexor hallucis longus.
Figure 5. A: anterior view of the medial recess of the ankle; B: the fibers of the deep tibiotalar ligament are tightened with the palpation probe.
Figure 6. Maneuvers to demonstrate ligament instability. A: lesion of the syndesmosis allowing insertion of the palpation probe into the distal tibiofibular zone; B: lesion of the deltoid ligament allowing insertion of the probe into the medial tibiotalar space.
Figure 7. A: debridement of the tibiofibular space; B: stabilization of the syndesmosis using a suspension system.
Información del artículo
Cita bibliográfica
Autores
Josep Torrent Gómez
Institut Rabat. Barcelona Foot and Ankle Clinic
Hospital QuirónSalud Barcelona
Minimally Invasive Foot and Ankle Surgery (MIFAS)
Servicio de Cirugía Ortopédica y Traumatología. Hospital Universitario Mútua de Terrassa. Terrassa. Barcelona
Cinthya Vargas Zavala
Unidad de Pie y Tobillo. Move. Barcelona. España
Servicio médico RCD Espanyol. Barcelona. España
Ethical responsibilities
Conflicts of interest. The authors declare that they have no conflicts of interest.
Financial support. This study has received no financial support.
Protection of people and animals. The authors declare that this research has not involved human or animal experimentation.
Data confidentiality. The authors declare that the protocols of their work centre referred to the publication of patient information have been followed.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Referencias bibliográficas
-
1Yuen CP, Lui TH. Distal Tibiofibular Syndesmosis: Anatomy, Biomechanics, Injury and Management. Open Orthop J. 2017;11:670-7.
-
2Ray RG. Arthroscopic Anatomy of the Ankle Joint. Clin Podiatr Med Surg. 2016;33(4):467-80.
-
3Mengiardi B, Pinto C, Zanetti M. Medial Collateral Ligament Complex of the Ankle: MR Imaging Anatomy and Findings in Medial Instability. Semin Musculoskelet Radiol. 2016;20(01):91-103.
-
4McCollum GA, Van Den Bekerom MPJ, Kerkhoffs GMMJ, et al. Syndesmosis and deltoid ligament injuries in the athlete. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1328-37.
-
5Wagener ML, Beumer A, Swierstra BA. Chronic instability of the anterior tibiofibular syndesmosis of the ankle. Arthroscopic findings and results of anatomical reconstruction. BMC Musculoskelet Disord. 2011;12(1):212.
-
6Golanó P, Vega J, De Leeuw PAJ, et al. Anatomy of the ankle ligaments: a pictorial essay. Knee Surg Sports Traumatol Arthrosc. 2010;18(5):557-69.
-
7Hermans JJ, Beumer A, De Jong TAW, Kleinrensink G. Anatomy of the distal tibiofibular syndesmosis in adults: a pictorial essay with a multimodality approach. J Anat. 2010;217(6):633-45.
-
8Dalmau-Pastor M, Malagelada F, Kerkhoffs GMMJ, et al. The anterior tibiofibular ligament has a constant distal fascicle that contacts the anterolateral part of the talus. Knee Surg Sports Traumatol Arthrosc. 2020;28(1):48-54.
-
9Cain JD, Dalmau-Pastor M. Anatomy of the Deltoid-Spring Ligament Complex. Foot Ankle Clin. 2021;26(2):237-47.
-
10Aicale R, Maffulli N. Rotational ankle instability: A current concept review. J Orthop Surg (Hong Kong). 2023;31(2):10225536231182347.
-
11Roemer FW, Jomaah N, Niu J, et al. Ligamentous Injuries and the Risk of Associated Tissue Damage in Acute Ankle Sprains in Athletes: A Cross-sectional MRI Study. Am J Sports Med. 2014;42(7):1549-57.
-
12Vancolen SY, Nadeem I, Horner NS, et al. Return to Sport After Ankle Syndesmotic Injury: A Systematic Review. Sports Health. 2019;11(2):116-22.
-
13Ogilvie-Harris DJ, Reed SC, Hedman TP. Disruption of the ankle syndesmosis: biomechanical study of the ligamentous restraints. Arthroscopy. 1994;10(5):558-60.
-
14Ribbans WJ, Garde A. Tibialis Posterior Tendon and Deltoid and Spring Ligament Injuries in the Elite Athlete. Foot Ankle Clin. 2013;18(2):255-91.
-
15Miller CD, Shelton WR, Barrett GR, et al. Deltoid and Syndesmosis Ligament Injury of the Ankle Without Fracture. Am J Sports Med. 1995;23(6):746-50.
-
16Hintermann B, Valderrábano V, Boss A, et al. Medial Ankle Instability: An Exploratory, Prospective Study of Fifty-Two Cases. Am J Sports Med. 2004;32(1):183-90.
-
17Sman AD, Hiller CE, Rae K, et al. Diagnostic accuracy of clinical tests for ankle syndesmosis injury. Br J Sports Med. 2015;49(5):323-9.
-
18Ashkani Esfahani S, Bhimani R, Lubberts B, et al. Volume measurements on weightbearing computed tomography can detect subtle syndesmotic instability. J Orthop Res. 2022;40(2):460-7.
-
19Tourné Y, Molinier F, Andrieu M, et al. Diagnosis and treatment of tibiofibular syndesmosis lesions. Orthop Traumatol Surg Res. 2019;105(8S):S275-S286.
-
20Chun KY, Choi YS, Lee SH, et al. Deltoid Ligament and Tibiofibular Syndesmosis Injury in Chronic Lateral Ankle Instability: Magnetic Resonance Imaging Evaluation at 3T and Comparison with Arthroscopy. Korean J Radiol. 2015;16(5):1096.
-
21Vega J, Allmendinger J, Malagelada F, et al. Combined arthroscopic all-inside repair of lateral and medial ankle ligaments is an effective treatment for rotational ankle instability. Knee Surg Sports Traumatol Arthrosc. 2020;28(1):132-40.
-
22Corte-Real N, Caetano J. Ankle and syndesmosis instability: consensus and controversies. EFORT Open Rev. 2021;6(6):420-31.
-
23Nichols JA, Baratta C, Reb CW. Biomechanical Sequelae of Syndesmosis Injury and Repair. Foot Ankle Clin. 2023;28(1):77-98.
-
24Rellensmann K, Behzadi C, Usseglio J, et al. Acute, isolated and unstable syndesmotic injuries are frequently associated with intra-articular pathologies. Knee Surg Sports Traumatol Arthrosc. 2021;29(5):1516-22.
-
25Gardner MJ, Graves ML, Higgins TF, Nork SE. Technical considerations in the treatment of syndesmotic injuries associated with ankle fractures. J Am Acad Orthop Surg. 2015;23(8):510-8.
-
26Miller AN, Barei DP, Iaquinto JM, et al. Iatrogenic syndesmosis malreduction via clamp and screw placement. J Orthop Trauma. 2013;27(2):100-6.
-
27Van Den Bekerom MPJ, Hogervorst M, Bolhuis HW, Van Dijk CN. Operative aspects of the syndesmotic screw: Review of current concepts. Injury. 2008;39(4):491-8.
-
28Grassi A, Samuelsson K, D’Hooghe P, et al. Dynamic Stabilization of Syndesmosis Injuries Reduces Complications and Reoperations as Compared With Screw Fixation: A Meta-analysis of Randomized Controlled Trials. Am J Sports Med. 2020;48(4):1000-13.
-
29Ræder BW, Figved W, Madsen JE, et al. Better outcome for suture button compared with single syndesmotic screw for syndesmosis injury: five-year results of a randomized controlled trial. Bone Joint J. 2020;102-B(2):212-9.
-
30Kingston KA, Lin Y, Bradley AT, et al. Salvage of Chronic Syndesmosis Instability: A Retrospective Review With Mid-Term Follow-Up. J Foot Ankle Surg. 2023;62(2):210-7.
-
31Ryan PM, Rodríguez RM. Outcomes and Return to Activity After Operative Repair of Chronic Latent Syndesmotic Instability. Foot Ankle Int. 2016;37(2):192-7.
-
32Gomaa AR, Mason L. Chronic syndesmotic instability – Current evidence on management. J Clin Orthop Trauma. 2024;50:102382.
-
33Stenquist DS, Ye MY, Kwon JY. Acute and Chronic Syndesmotic Instability. Clin Sports Med. 2020;39(4):745-71.
-
34Colin F, Barbier O, Cordier G. Role of surgery in the management of lesions of the medial collateral ligament of the ankle. Orthop Traumatol Surg Res. 2020;106(8S):S195-S199.
-
35Brady AW, Bryniarski A, Brown JR, et al. The Biomechanical Role of the Deltoid Ligament on Ankle Stability: Injury, Repair, and Augmentation. Am J Sports Med. 2023;51(10):2617-24.
-
36Loozen L, Veljkovic A, Younger A. Deltoid ligament injury and repair. J Orthop Surg (Hong Kong). 2023;31(2):10225536231182345.
-
37Kim SH, Lee SH, Cha JY, et al. Arthroscopic Deltoid Ligament Repair as a Potential Alternative Treatment for Ankle Deltoid Ligament Injury. J Clin Med. 2025;14(5):1662.
-
38Guelfi M, Vega J, Malagelada F, Dalmau-Pastor M. Arthroscopic repair of the tibiotalar fascicle of deltoid ligament is feasible through anterior ankle arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2024;32(12):3105-11.
-
39Savage-Elliott I, Murawski CD, Smyth NA, et al. The deltoid ligament: an in-depth review of anatomy, function, and treatment strategies. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1316-27.
Descargar artículo:
Licencia:
Este contenido es de acceso abierto (Open-Access) y se ha distribuido bajo los términos de la licencia Creative Commons CC BY-NC-ND (Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional) que permite usar, distribuir y reproducir en cualquier medio siempre que se citen a los autores y no se utilice para fines comerciales ni para hacer obras derivadas.
Comparte este contenido
En esta edición
- Anterior ankle arthroscopy at its best
- Foot and ankle arthroscopy, a consolidated and expanding reality
- The history and current concepts of ankle arthroscopy
- Current status of anterior ankle impingement
- Arthroscopic treatment of chronic lateral ankle instability
- Managing osteochondral lesions of the talus with anterior ankle arthroscopy
- Role of arthroscopy in syndesmosis injuries
- Role of arthroscopy in the treatment of ankle fractures
- Anterior arthroscopic ankle arthrodesis
- The use of needle arthroscopy in the ankle
- The letter pi on the ankle
Más en PUBMED
Más en Google Scholar
Más en ORCID


Revista Española de Artroscopia y Cirugía Articular está distribuida bajo una licencia de Creative Commons Reconocimiento-NoComercial-SinObraDerivada 4.0 Internacional.